Adam Benton/Kromekat Digital Art & Design

In 1895 two French physicians attempted a radical departure from the standard cancer treatment regimen. Instead of surgery, Charles Richet and Jules Hericourt administered an antiserum derived from dogs to patients with advanced cancer.1 Some patients improved, although significant immunogenicity problems occurred. Lacking specificity and purity, the formulation cured no one.
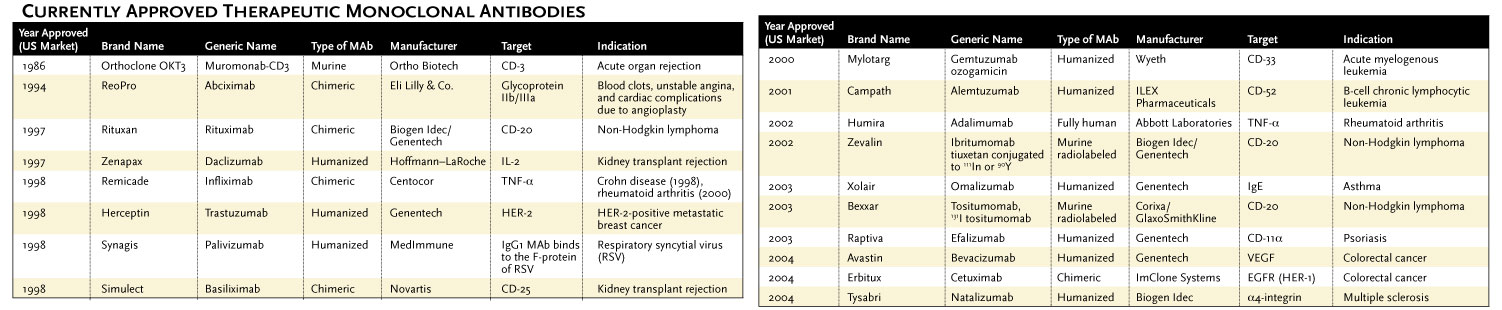
Now, after a century of setbacks and intermittent successes, therapeutic antibodies – or more specifically, therapeutic monoclonal antibodies (MAbs) – are finally coming into their own. More than 100 such drugs are in clinical trials, and 18 have been approved for use in the United States. Those therapies generated between $5 billion and $6 billion in revenue in 2003, a number that is predicted to triple in the next five years. By one estimate, MAbs will account for 32% of all revenues in the biotech market by 2008.2
"We're really unraveling...
FROM MOUSE TO HUMAN
Milstein and Köhler shared (with Niels Jerne) the Nobel Prize in medicine in 1984, nine years after their breakthrough. But it would be another 13 years before a drug manufacturer was able to parlay hybridoma technology into an anticancer drug that would pass US Food and Drug Administration (FDA) muster. That drug was Rituxan (rituximab), an antibody to the B-cell marker CD-20 that is intended to combat non-Hodgkin lymphoma.
Paradoxically, the delay is largely attributable to the recipients' immune systems, which recognized the antibodies – produced in mice – as foreign and inevitably attacked them.
"Mouse MAbs never really proved to be very successful therapeutics for chronic indications, because they were highly antigenic," says Alejandro Aruffo, president of the Abbott Bioresearch Center and Immunoscience Development Center at Abbott Laboratories in Boston. "A single dose triggered a strong immune system response that neutralized the activity of the antibodies."
Several rounds of "humanization" ensued, in which researchers tried to reengineer the mouse antibodies to make them ever more human. First, using recombinant DNA technology, scientists fused the mouse variable regions (VH and VL) to the human immunoglobulin (Ig)-constant domain. Two-thirds human and one-third mouse, these chimeric molecules substantially alleviated human-anti-mouse antibody (HAMA) responses, yet they still produced unwanted immune activity. The chimeric drugs Rituxan and Remicade (infliximab), for example, have been associated with serious allergic reactions.
Next, scientists inserted just the mouse complementary-determining regions (CDRs) – those regions of the antibody that bind antigen – into a human antibody framework. The resulting "humanized" antibodies (90% to 95% human) produced far fewer HAMA responses but did not eliminate them. Other drawbacks were also evident: Designing humanized antibodies is technically demanding, and humanization can produce antibodies with reduced affinities for their targets.
FULLY HUMAN ANTIBODIES
Manufacturing hurdles and the persistence of adverse immune effects among certain chimeric and humanized MAbs have sparked an effort to create fully human antibodies, which promise to evade the human immune response. Scientists have developed two different approaches to the problem: Either they can change the mouse, or avoid it all together.
Abgenix of Fremont, Calif., was the first company to turn an ordinary mouse into a human antibody factory. Called XenoMouse, it is a transgenic animal in which native antibody genes have been replaced with their human counterparts. Abgenix has used the platform both for internal drug development and in partnership with other drug developers, including Amgen in Thousand Oaks, Calif., Human Genome Sciences in Rockville, Md., and Chiron in Emeryville, Calif. According to Abgenix's Web site, 11 XenoMouse-generated antibodies have moved into clinical trials, including ABX-EGF (panitumumab), an anticancer drug targeting the epidermal growth-factor receptor. Developed in partnership with Amgen, panitumumab is currently in Phase II trials for metastatic colorectal cancer.
Medarex, based in Princeton, NJ, has also developed a fully human transgenic mouse platform. Medarex's HuMab-Mouse technology allows for faster production of fully human MAbs. "It's simple and straightforward," says company president and CEO Don Drakeman. The company and its partners have more than 150 fully human MAbs in development, including MDX-010, an anti-CTLA-4 compound now in Phase III clinical trials for metastatic melanoma. The drug is being developed in collaboration with Bristol-Myers Squibb.
UK-based Cambridge Antibody Technology skips the mouse altogether, isolating human monoclonal antibodies via a test tube-based phage-display system instead. Phage display reduces antibody production time from months to weeks. "It is somewhat like fishing," explains David Glover, chief medical officer. "You have a pool of antibodies and go fishing with the antigen as the bait. Some antibodies will bite; the ones that don't are thrown away. You sort your catch to find the ones that bind the best and have the highest specificity." The company houses a library of more than 100 billion distinct phage antibodies.
Eleven human MAbs originating at Cambridge Antibody Technology have entered clinical trials, including Humira (adalimumab), the first fully human MAb approved for sale in the US. Developed in collaboration with Abbott and targeting tumor necrosis factor (TNF)-a, Humira was approved for the treatment of rheumatoid arthritis in 2002 and is currently being investigated for other inflammatory diseases; it garnered $852 million in sales in 2004.
Cambridge, Mass.-based Dyax has an automated phage-display discovery tool that allows scientists to rapidly select the best antibody, small protein, or peptide binders from libraries containing billions of candidates. "We have a speed and throughput that is greater than the vast majority of hybridoma-based approaches," says Clive Wood, Dyax's chief scientific officer. "We can select, in a short period, antibodies that bind with a potency and selectivity that outstrips what medicinal chemists can normally achieve."
Human Genome Sciences also houses it own collection of proprietary antibody targets. In 2000, the company purchased rights to technology that allows it to produce human antibodies for clinical trials without the help of an outside pharmaceutical company. The company's human MAb, LymphoStat-B (isolated at Cambridge Antibody Technology), recognizes and inhibits the B-lymphocyte stimulator, typically found in high levels among patients with lupus and rheumatoid arthritis.
On February 1, 2005, MorphoSys, based near Munich, Germany, announced that the first fully human therapeutic candidate based on its HuCAL technology entered clinical trials in Europe. Munich-based GPC Biotech is conducting the Phase I trial of ID09C3, an anti-MHC class II monoclonal, in patients with B-cell lymphomas. MorphoSys' HuCAL GOLD combinatorial library contains more than 10 billion members; therapeutic candidates are selected using phage display.
MONOCLONALS FOR CANCER
Therapeutic MAbs have opened a completely new field of biomedical research and have clearly illustrated the immune system's power to fight chronic disease, especially cancer. "MAbs really represent the first concerted examples of success in targeted therapy," says Louis M. Weiner, chair of the department of medical oncology at Fox Chase Cancer Center in Philadelphia. "They have forced researchers and clinical oncologists to change their thinking. Instead of blowing apart a cancer's DNA with classical chemotherapy, cancer biology is telling us where to attack."
Now some drug developers are moving beyond the standard antibody molecule structure to improve both potency and effectiveness. The approach involves conjugating "payloads" – for example, chemotherapeutic agents, radioactive particles, or other toxins – to the antibodies. And it gives oncologists the ability to target highly toxic treatments precisely where they are needed. Some say this is the only means to move therapeutic MAbs into the future.
In 2002, Cambridge, Mass.-based Biogen Idec's (formerly IDEC Pharmaceuticals) Zevalin (90Y ibritumomab tiuxetan) became the first radioimmunoconjugate approved for cancer treatment. It combines the chimeric antibody Rituxan with the metal chelator, MD-DTPA, which provides stability when used for radionucleotide tumor imaging and chemotherapy. Because murine-oriented MAbs exit the body faster than those with a higher human content, the chimeric Zevalin offers a rare advantage: It allows for swift removal of radiation from the body.
Earlier this month the
But therapeutic antibodies aren't just for cancer. Last November, the FDA approved Biogen Idec's natalizumab (Tysabri, formerly Antegren), a humanized MAb for the treatment of multiple sclerosis. MAbs targeting immunoglobulin, such as Genentech's omalizumab (Xolair), have had an enormous impact on the treatment and management of asthma and other inflammatory diseases. Unlike standard asthma therapies that treat symptoms, MAbs for asthma target the underlying cause. Cambridge Antibody Technology's CAT-354, a human anti-IL-13 monoclonal antibody for the treatment of severe asthma, is in early-stage clinical trials. Other human antibodies targeting inflammation include Abbott's ABT-874, an IL-12 inhibitor for the treatment of multiple sclerosis and other autoimmune diseases, and ABT-328, an IL-18 inhibitor for lupus.
FUTURE CHALLENGES
Fully human MAbs have significantly improved efficacy and reduced toxicity, but roadblocks remain. Anti-TNF-a agents such as Humira have been associated with an increased risk of infection, including tuberculosis. And while MAbs are revolutionizing cancer care, they are not applicable to all patients, as only some tumors overexpress the receptor or antigen of interest. Tumors can also shed the desired antigen into the bloodstream, essentially putting MAb therapy onto an unproductive detour that never reaches the cancer site.
Other drawbacks are apparent. One is that MAbs can't enter cells; they attach to proteins or molecules only on the surface. This limits the number of targets one can pursue and, thus, the types of diseases that can be treated. InNexus Biotechnology of Vancouver, British Columbia, has addressed that problem with its so-called SuperAntibody Technology (SAT).
InNexus' SAT platforms combine site-specific chemical conjugation and genetically engineered fused proteins to improve MAb potency, avidity, and affinity, and promote intracellular transit. Early proof-of-principle studies suggest that coupling a synthetic peptide, called a membrane-translocator sequence, to an MAb allows it to penetrate cells and target antigens from within.5 The company is now developing SuperAntibody conjugates for the treatment of plaque associated with coronary artery disease.
The cost of MAb therapeutic agents is also a concern. Drug developers often must pay royalties to those who hold key intellectual property in MAb production and target identification. Such payments can mean considerable cash for the companies holding the patents, but for pharmaceutical companies marketing a drug based on someone else's platform, it can be a financial burden, and one that inevitably is passed onto the patient.
Moreover, drugs currently must be injected. Technology for making oral or inhaled formulations could come sometime in the future, says Medarex's Drakeman, but "it's not there yet."
Perhaps the biggest challenge facing antibody developers today lies in maintaining a full drug pipeline. Five years ago, with the decoding of the human genome, the number of potential therapeutic targets seemed limitless. But in practice, working with the new targets provided by the Human Genome Project is proving to be difficult and taking longer than expected.
Few clinically validated targets have been identified, says Glover. "In terms of when there will be enough good-quality targets to make good antibodies against them is a difficult question," he explains. "After this present flush of antibodies, there will be new targets that come along, and there may be ways to improve, but one could argue that the major growth phase has already passed."
Not everyone agrees. "There are thousands of more targets that have not been appreciated," says Ivor Royston, a pioneer in the field of monoclonal antibodies and a managing member of San Diego-based Forward Ventures. "I believe MAbs will be the single, fastest growing sector of biopharmaceuticals for the indefinite future," says Drakeman.
Whatever the case, 30 years after their invention, monoclonal antibodies have finally established a firm beachhead in the clinic. "What we're really seeing now is an understanding of how to use these agents," says Abbott's Aruffo. "For a long time people were skeptical about whether they could deliver on their promise. Now, with MAbs like Humira, we see they can be used for chronic disease, and provide a lot of patient benefit."
Interested in reading more?
