 Cisplatin crystalsFLICKR, KAT M RESEARCH
Cisplatin crystalsFLICKR, KAT M RESEARCH
When cancer cells are first discovered, many drugs can blast them into oblivion. But over time, cancers begin to withstand those first line drugs and continue to grow and spread.
“If you already have 1010 tumor cells, the chances are you’re going to have some kind of resistance develop,” said William Pao, a physician scientist at Vanderbilt University, who first uncovered mechanisms of drug resistance in lung cancer. “Even if you kill 99.9 percent of cells you’re still left with a ton of cells which then can start to grow.”
A long-standing hurdle in cancer therapy, researchers are now making inroads into understanding how cancer cells acquire drug resistance, and they’re finding that genetic mutations are just one of many strategies cancers use to evade death. Cancer cells have been found to boost transcription of survival genes, drill out the cores of...
Genetic changes
Each of the many cancer cells in a tumor can have slight genetic variations. While the vast majority of cells in a tumor may be susceptible to a drug, a few cells can harbor mutations that allow it to withstand the toxic assault. Over time, all the susceptible cells die off, while those which are resistant proliferate.
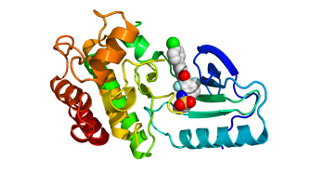
This selective pressure allows breast and other cancers to acquire resistance to the platinum-based chemotherapy drug Cisplatin. In 1996, researchers found that some cancer cells developed mutations that enable them to literally pump the drug out of the cytoplasm, thus allowing the cells to withstand higher and higher doses without dying, said David Solit, an oncologist at Memorial Sloan-Kettering Cancer Center in Boston.
Similarly, as pharmaceutical companies developed a class of drugs called kinase inhibitors that blocked key molecules in cell division pathways known to be hyperactive in a variety of cancers, tumors began to develop mutations that allowed them to divide in the absence of those molecules. Some cancers, including lung cancer, even evolved to no longer depend on the division pathway at all, making any type of drug that targeted that pathway ineffective, Pao said.
Epigenetic changes
In addition to genetic mutations, researchers are finding that epigenetic changes may also allow cancer cells to nimbly respond to drugs. Unlike mutations, epigenetic changes can occur more quickly in response to environmental changes, said Pamela Munster, an oncologist and hematologist at the University of California, San Francisco.
Last month, Munster and her colleagues published that epigenetic changes are responsible for the resistance many breast cancers acquire against the estrogen blocking drug Tamoxifen after around 18 months of treatment. When the researchers looked at the genetic profile of the breast cancer cells, they didn’t find any mutations that correlated with resistance, but found that resistant lines were transcribing a survival gene called Akt at much higher levels than susceptible cells. The cancer cells used histone tags, or chemical markers on the chromatin, to expose the Akt gene and increase its transcription. The higher Akt signal allowed cancer cells to stay alive even in the presence of the drug by stimulating growth and proliferation and preventing cell death.
“What we learned is the tumor cells have a way of tagging the genes with the resistance marker that they can then pass on to other generations,” Munster said, giving those cells’ progeny an advantage in the drug-treated environment.
Cancer cells may also take a page from viruses to switch between resistance and susceptibility, according to a study published November 9 in the American Journal of Pathology. D. Stave Kohtz, a molecular biologist at the Mount Sinai School of Medicine in New York, and his colleagues were studying why ovarian carcinomas sometimes become resistant to a drug, only to become susceptible again after the drug is no longer taken. Such a change is unlikely to be caused by genetic mutations, because those are usually not reversible so quickly, Kohtz said.
Prior studies had shown that nuclear pores, which help transport nuclear elements to the cytoplasm and vice versa, could influence gene expression by interacting with chromatin at the periphery of the nucleus. Specifically, nuclear pores can activate transcription by shielding DNA from repressors, or hinder transcription because repressor proteins lurk in the region near the nuclear boundary. Given their influence on gene expression, Kohtz and his colleagues wondered if nuclear pores might be altered in different cancer cell types.
Using electron microscopy to visualize the nuclei of cancer cells resistant to the drug Cisplatin, the researchers saw that the nuclear pores “didn’t look right,” Kohtz said. They appeared to be hollow, he said, with a key gatekeeper protein in the center disassembled—similar to pores affected by viruses that co-opt cellular transport machinery for its own purposes. When the team knocked out the cores of nuclear pores in other cancer cells, they found the cells were frozen in an early stage of cell division. These hibernating cells didn’t grow very much, but they were also resistant to Cisplatin. Kohtz believes these sleeper cells can lie in wait, resisting the toxic effects of drug therapy, until some other signal turns them on.
“In vivo, the idea is that they will sit at metastatic sites or even in the region of the original tumor until something wakes them up and makes them start growing again,” Kohtz said.
Alternative splicing
Yet another way cancers can acquire drug resistance has to do with protein processing. Between 40 to 80 percent of melanoma patients have a mutated BRAF gene, which turns on cellular growth and division signaling pathway, Solit said. Last year, drug maker Plexxicon showed that a compound targeting mutant forms of BRAF, called Vemurafenib, significantly lengthened lives in melanoma patients with the mutation.
Vemurafenib exploits the fact that BRAF proteins in healthy cells pair up with other BRAF proteins to form a multiprotein complex, while the mutated BRAF protein act as a lone compound. This solitary structure can be hundreds of times more effective in activating cell division than the normal paired BRAF complexes, said co-author Roger Lo, a dermatologist at the University of California, Los Angeles, who studies skin cancer. Vemurafenib targets tumor cells by only inhibiting the standalone mutant version, while allowing the twinned version in healthy cells to act unimpaired.
But within 18 months, many patients develop resistance to Vemurafenib, and their tumors progress. To understand why, Solit and his colleagues looked at resistant cancer cell lines and found “some of the resistant cells generate a variant form of BRAF” that is shorter, he said. But the shorter BRAF protein wasn’t made by a mutation in a protein coding region of DNA, according to a paper published last Wednesday (November 23) in Nature. Instead, deletions of exon regions of the gene led to alternative splicing that generated the shorter version, which can bind to itself, rendering the protein undetectable by Vemurafenib.
Tackling resistant cancers
While cancer cells use an intimidating array of tactics to evade drug therapies, researchers are slowly developing ways to target resistant cells. In human trials, Munster’s team has found that adding a compound that removes histone tags to the Tamoxifen regimen can make resistant breast cancers sensitive to the drug once again. Similarly ongoing Phase II trials are testing the combination of Vemurafenib and another drug that inhibits a compound in the same the cellular division pathway in melanoma patients resistant to Vemurafenib. And for those cancers that have switched between quiescence and active growth, simply retreating with the same medicine later on can sometimes be effective, Kohtz said.
While there may be general principles that apply to cancer resistance, for now, treatment requires a tailored approach that uses frequent biopsies of tumors to see what genetic and epigenetic mutations they’ve acquired, Pao said. With more thorough genetic sequencing, it’s become clear that there’s no single answer, even for a single patient.
“We’re all looking for the common theme, so that we can find ways to overcome it,” Pao said. Unfortunately, “cancers are heterogeneous, not just across individuals, but within individuals.”
Interested in reading more?




