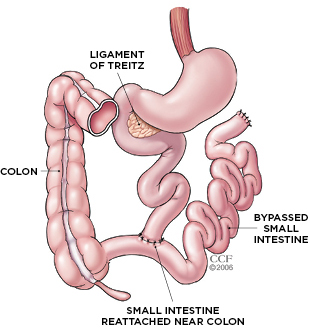
 CUT-AND-PASTE GI TRACT: The intestine is divided into three segments: the duodenum, the jejunum, and the ileum. Surgeons performing jejunoileal bypass surgery would sever the small intestine in the jejunal region, about 35 cm below its attachment to the ligament of Treitz. The cut end was then sewn into an area of the ileal segment, about 10 cm from its natural attachment to the large intestine, or colon. As a result, about 90 percent of the small bowel was bypassed, greatly limiting micronutrient absorption. The remaining section of small intestine itself rarely caused any problems, but patients who underwent the procedure suffered severe malnutrition, often leading to organ failure and death. CLEVELAND CLINICIn 2009, Dushyant Singh, a gastroenterologist at Overland Park Regional Medical Center in Shawnee, Kansas, met a 64-year-old man with advanced liver disease, as well as a long history of kidney stones, progressive kidney disease, arthritis, diarrhea, fatigue, joint pain, slurred speech, and other concerning symptoms. His case was peculiar, and doctors could not pinpoint the cause of his deteriorating condition. The patient eventually mentioned having had “weight-loss surgery” in the mid-1970s, but upper endoscopy showed no sign of a modern gastric-bypass procedure. Singh wondered if the patient had undergone jejunoileal bypass, a once wildly popular weight-loss surgery that was later discovered to cause a slew of health problems, some fatal (World J Gastroenterol, 15:2277-79, 2009).
CUT-AND-PASTE GI TRACT: The intestine is divided into three segments: the duodenum, the jejunum, and the ileum. Surgeons performing jejunoileal bypass surgery would sever the small intestine in the jejunal region, about 35 cm below its attachment to the ligament of Treitz. The cut end was then sewn into an area of the ileal segment, about 10 cm from its natural attachment to the large intestine, or colon. As a result, about 90 percent of the small bowel was bypassed, greatly limiting micronutrient absorption. The remaining section of small intestine itself rarely caused any problems, but patients who underwent the procedure suffered severe malnutrition, often leading to organ failure and death. CLEVELAND CLINICIn 2009, Dushyant Singh, a gastroenterologist at Overland Park Regional Medical Center in Shawnee, Kansas, met a 64-year-old man with advanced liver disease, as well as a long history of kidney stones, progressive kidney disease, arthritis, diarrhea, fatigue, joint pain, slurred speech, and other concerning symptoms. His case was peculiar, and doctors could not pinpoint the cause of his deteriorating condition. The patient eventually mentioned having had “weight-loss surgery” in the mid-1970s, but upper endoscopy showed no sign of a modern gastric-bypass procedure. Singh wondered if the patient had undergone jejunoileal bypass, a once wildly popular weight-loss surgery that was later discovered to cause a slew of health problems, some fatal (World J Gastroenterol, 15:2277-79, 2009).
Doctors first began offering jejunoileal bypass, one of the earliest bariatric surgeries, in the late 1960s, after surgeons noticed that patients who had lost a portion of their small intestine would lose weight, even as they ate more. The procedure involved bypassing about 90 percent of the small intestine to short-circuit nutrient absorption. And it worked. Patients immediately started shedding pounds. More than 100,000 overweight people chose to undergo the surgery. “Every decade has a new fashion,” says Singh. “[Jejunoileal bypass] was the fashion statement in the early ’70s. Everybody was getting this.”
But in addition to absorbing fewer calories from the food they ate, jejunoileal bypass patients were also absorbing fewer micronutrients. Soon, they began having trouble seeing at night because they became deficient ...
















