© MOLLY MENDOZA
© MOLLY MENDOZA
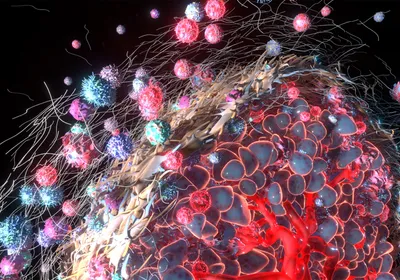
Cancer is a scourge of humanity, and one that will affect more and more people as life spans increase. Approximately one in three people is struck by neoplastic disease in his or her lifetime. But, the other side of that coin is that two out of three people remain unaffected. Even the majority of heavy smokers, who bombard their lungs with carcinogens and tumor promoters over many years, remain cancer free. Naturally, the suffering of cancer patients and their families has inspired researchers to study the cellular changes unique to cancer and the genetics of cancer susceptibility. The genetics of cancer resistance, as a topic in its own right, has remained largely unexplored.
Pathologists have shown that virtually all men age 60 or older have ...