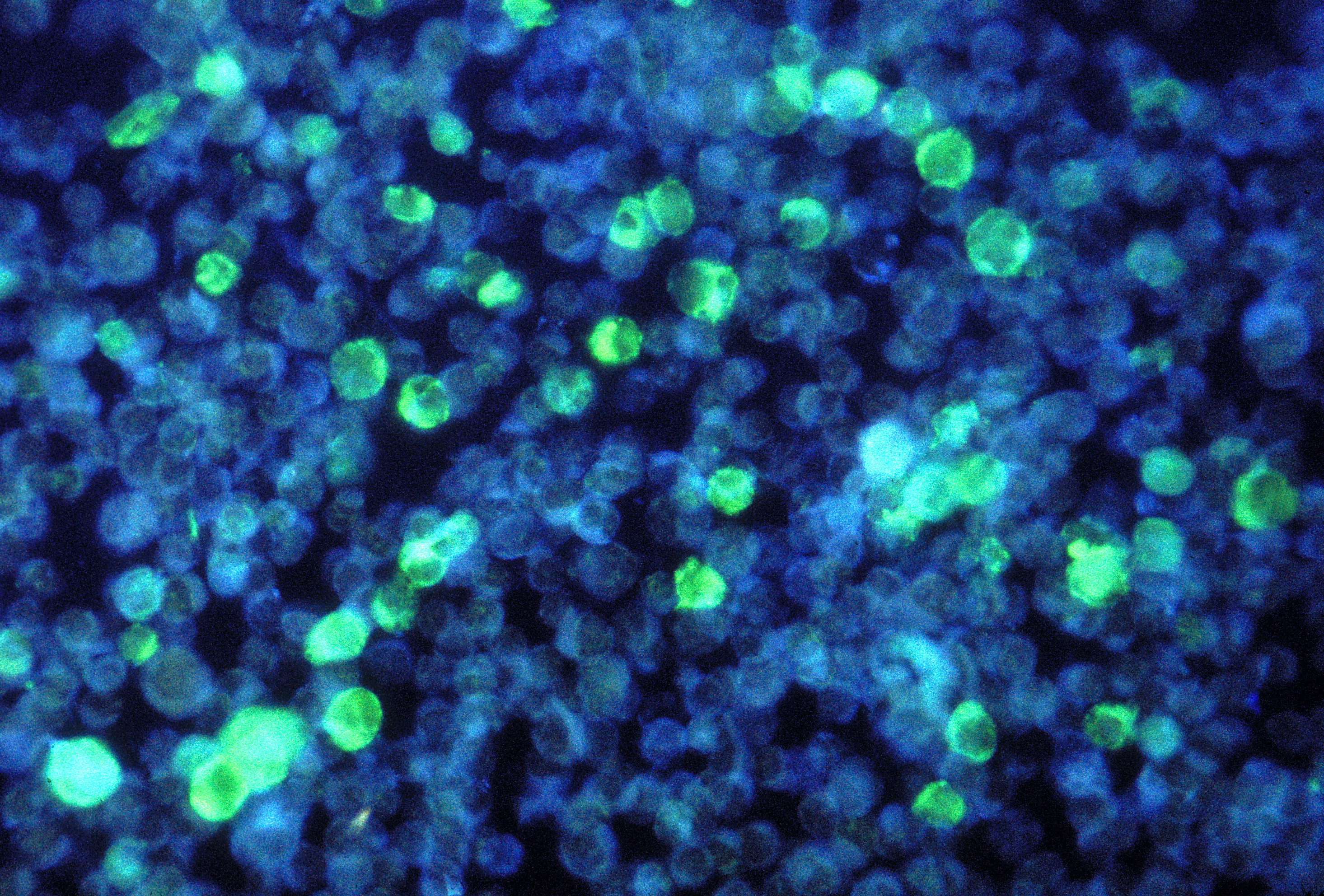
 Leukemia cells containing Epstein-Barr VirusCDC, PAUL M. FEORINO
Leukemia cells containing Epstein-Barr VirusCDC, PAUL M. FEORINO
When Epstein-Barr virus (EBV) causes cancer, it usually does so by hijacking two cellular mechanisms. First, the virus deregulates MYC so that B cells can rapidly replicate. Then, the virus overrides the B cell’s built-in failsafe—programed cell death—by silencing an apoptotic gene, BCL2L11 (Bim). Now, in a November 10 study published in eLIFE, researchers describe one mechanism by which EBV controls the expression of these genes.
The two genes are “really important in cancer development,” said coauthor Michelle West, a biochemist at the University of Sussex, U.K. “We know the virus produces proteins that control these genes. We were interested in understanding how it turns on MYC and switches off another gene called BCL2L11.”
EBV, one of the first oncoviruses discovered, infects more than 90 ...



















