 ISTOCK, SAEMILEEThe flu is dominating the U.S. It is now widespread in 49 states and Puerto Rico and has sickened thousands since October, the Centers for Disease Control and Prevention reports. Tens of thousands die each year as a result of the flu.
ISTOCK, SAEMILEEThe flu is dominating the U.S. It is now widespread in 49 states and Puerto Rico and has sickened thousands since October, the Centers for Disease Control and Prevention reports. Tens of thousands die each year as a result of the flu.
“We need to make the universal flu vaccine a higher priority than it has been,” Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases (NIAID), tells The Scientist.
Researchers have long sought a flu vaccine that would protect individuals season after season with just a single inoculation, similar to the measles or chickenpox vaccines. But unlike the measles or chickenpox virus, which are both fairly stable in genetic structure, the influenza virus has many rapidly mutating strains. And because the strains mutate so quickly, making them unrecognizable to the body’s immune system, a new flu vaccine has to be developed each year or every other year.
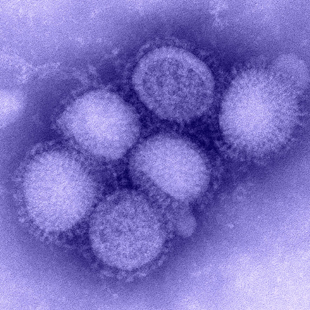 Micrograph of H1N1 virusCDC INFLUENZA LABORATORY
Micrograph of H1N1 virusCDC INFLUENZA LABORATORY





















