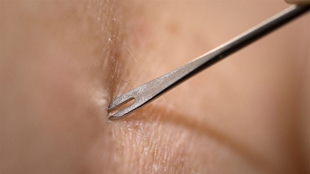
 Small vaccine deliveryJAMES GATHANY, CDC
Small vaccine deliveryJAMES GATHANY, CDC
The smallpox vaccine was the first, and arguably most successful, vaccine ever put into practice, and it was scratched into the skin of individuals. With the invention of syringes and hypodermic needles, vaccination shifted toward administration directly into the muscle, under the assumption that it is better to get a vaccine straight into the body. But it turns out scientists may have had it right the first time.
A paper published this week in Nature suggests that the most important part of the human immune system actually resides in peripheral tissues, and that vaccination through those tissues may be more effective than traditional vaccination into the muscle.
The finding is “quite remarkable,” said Onur Boyman, an immunologist at the University of Zurich, who was not ...

















