Alzheimer’s disease is characterized by the accumulation of amyloid β (Aβ) peptides and the protein Tau in neurons in the brain. As a result, researchers focused on the central nervous system to study this disorder and its possible treatments. However, recent studies point to correlations between Alzheimer’s disease and alterations in peripheral organ systems, including the gut microbiome.1,2 Still, researchers do not completely understand if these peripheral disruptions are caused by the neurodegeneration or if they augment the existing disease symptoms.
To address this, two teams led by geneticists Hugo Bellen and Hongjie Li at the Baylor College of Medicine profiled the fly transcriptome in an Alzheimer’s disease model.3 The teams identified distinct effects from Aβ peptides and Tau in the central nervous system and peripheral tissue, respectively. Aβ particularly affected sensory neurons, while Tau induced aging phenotypes in peripheral tissues.
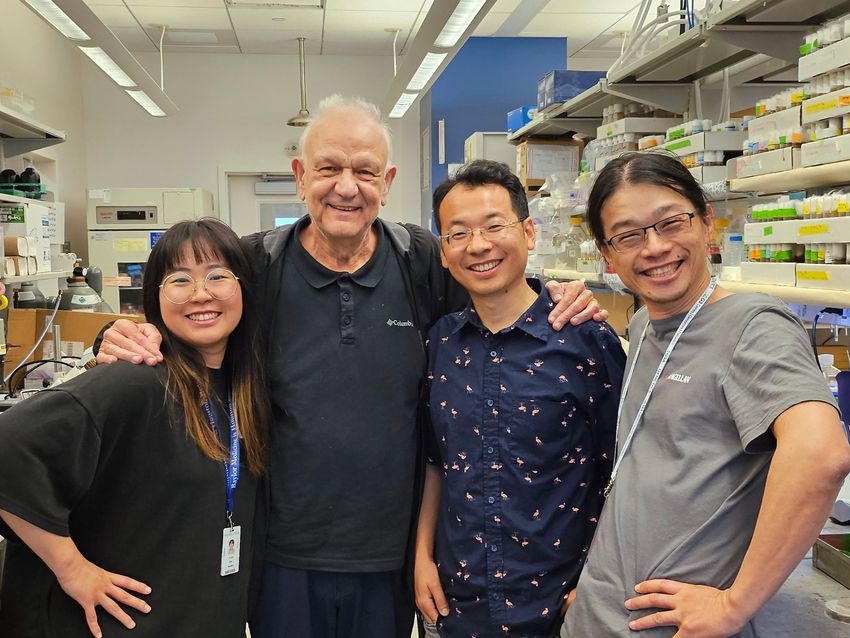
Researchers at the Baylor College of Medicine developed an Alzheimer’s disease fly cell atlas to study whole body effects of the neurodegenerative disorder. From left to right: Ye-Jin Park, Hugo Bellen, Hongjie Li, and Tzu-Chiao Lu.
Lindsey Goodman
The findings, published in Neuron, improve the understanding of Alzheimer’s disease pathogenesis. “It’s more [of] an exploratory study, but it creates a lot of useful information that can be mined,” Bellen said.
Malú Tansey, a neuroscientist at Indiana University who was not involved with the study, said the findings were exciting. “Even though it's a fly, you're actually seeing the potential effect that too much of something could do to peripheral tissues or to other tissues in the brain,” she said.
For their study, the teams expressed either Tau or Aβ42, a peptide that contributes to plaques in Alzheimer’s disease, selectively in adult fly neurons using a controllable gene expression system.4 At selected time points, the researchers separated the heads and bodies of flies and studied transcriptional changes in the cells from these tissues using single-nucleus RNA sequencing. By referencing existing fly cell atlases, the team identified 219 cell types in their data set.
They observed that only Aβ42 peptide caused neuronal death in the central nervous system, with sensory neurons displaying the most susceptibility to this effect. To explore how Aβ42 caused neuron loss, the teams investigated gene expression profiles in these cells and identified a cell cluster with increased expression of the gene for lactate dehydrogenase (Ldh).
Studying this Ldh-expressing population further, the teams observed that this cluster had more transcripts related to endoplasmic reticulum stress and apoptosis. They also observed that auditory sensory neurons expressed the endoplasmic stress response genes earlier than other Ldh-expressing cells.
To extend their findings to mammals, the teams analyzed preexisting data sets from a murine model of Alzheimer’s disease and human neuron tissues.5-7 They identified Ldh-expressing clusters in both species. Human neurons also had higher expression of genes related to endoplasmic reticulum stress in this cluster.
“Since it’s a conserved phenomenon, we think this is highly associated with the disease progression,” said Tzu-Chiao Lu, a postdoctoral researcher in Li's group and study coauthor. “But what’s the meaning of such a neuron? It’s kind of a black box right now.” Lu hopes to continue exploring these neurons and their role in neurodegeneration progression.
In contrast to the central nervous system, inducing the expression of Tau in fly neurons altered gene expression in peripheral tissues, with the most affects in functions like fat metabolism, digestion, and reproduction. To examine the potential defects in fat metabolism experimentally, the researchers studied the size of lipid droplets in flies’ fat stores.
Whereas neuronal Tau expression increased the droplet size early in the disease, the droplet size reduced later on, pointing to dysregulated lipid metabolism as a result of Tau expression. The researchers also observed reduced numbers of mature cells in the gut epithelium, indicating dysregulated gut homeostasis.
These features, coupled with decreased reproduction in male flies, pointed to Tau-induced accelerated aging. By studying the number of transcripts per cell over time—an established marker of fly aging—and comparing these values between cells from control and Aβ42 or Tau-expressing flies, the researchers showed that cells from flies with Tau expression resembled that of older control flies.8
“We never expected this kind of huge peripheral aging in Tau overexpressing flies,” said Ye-Jin Park, a graduate student in Li's and Bellen’s groups and study coauthor. Park is interested in exploring more brain-body communication mechanisms, in particular in mouse models.
Tansey said that she would be interested in seeing how neuronal Tau expression affects immune exhaustion markers as another peripheral system to study the effects of accelerated aging. “My hope is that everybody who cares about brain health and studies Alzheimer's and Parkinson's and neurodegenerative diseases will start to collect more peripheral bio samples,” she said, calling them a “window into the brain.”
- Xiong J, et al. FSH blockade improves cognition in mice with Alzheimer’s disease. Nature. 2022;603(7901):470-476.
- Vogt NM, et al. Gut microbiome alterations in Alzheimer’s disease. Sci Rep. 2017;7(1):13537.
- Park Y-J, et al. Distinct systemic impacts of Aβ42 and Tau revealed by whole-organism snRNA-seq. Neuron. 2025.
- Iijima K, et al. Dissecting the pathological effects of human Aβ40 and Aβ42 in Drosophila: A potential model for Alzheimer's disease. Proc Natl Acad Sci USA. 2004;101(17):6623-6628.
- Haney MS, et al. APOE4/4 is linked to damaging lipid droplets in Alzheimer’s disease microglia. Nature. 2024;628(8006):154-161.
- Zhou Y, et al. Human and mouse single-nucleus transcriptomics reveal TREM2-dependent and TREM2-independent cellular responses in Alzheimer’s disease. Nat Med. 2020;26(1):131-142.
- Mathys H, et al. Single-cell atlas reveals correlates of high cognitive function, dementia, and resilience to Alzheimer’s disease pathology. Cell. 2023;186(20):4365-4385.e27.
- Lu T-C, et al. Aging Fly Cell Atlas identifies exhaustive aging features at cellular resolution. Science. 2023;380(6650):eadg0934.















