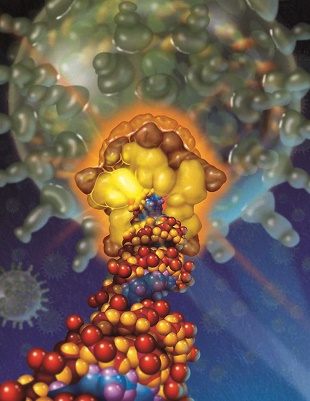
 PLOS BIOLOGY, PRECISION GRAPHICS, AATHAVAN AND CHEMLAThe search for alternatives to antibiotics has led many scientists to a treatment practice that’s been on the fringes of modern medicine for nearly a century. Bacteriophages—viruses that infect and kill bacteria—were first used in 1919 to treat a wide range of infections.
PLOS BIOLOGY, PRECISION GRAPHICS, AATHAVAN AND CHEMLAThe search for alternatives to antibiotics has led many scientists to a treatment practice that’s been on the fringes of modern medicine for nearly a century. Bacteriophages—viruses that infect and kill bacteria—were first used in 1919 to treat a wide range of infections.
Phage therapy fell out of favor with the advent of antibiotics; the practice has only persisted in some European countries as an experimental treatment. However, earlier this year, phage therapy was highlighted as one of seven approaches to “achieving a coordinated and nimble approach to addressing antibacterial resistance threats” in a 2014 status report from the National Institute of Allergy and Infectious Diseases (NIAID).
Classically, the treatment uses a bacteriophage, or cocktail of several phages, to specifically lyse target pathogenic bacteria. Researchers and biotech companies continue to refine this method, but in the absence of clear regulatory and manufacturing practices—and potential profits—phage therapy has yet to become mainstream for “the same reason many big companies have gotten out of making new antibiotics,” said microbiologist Jason ...















