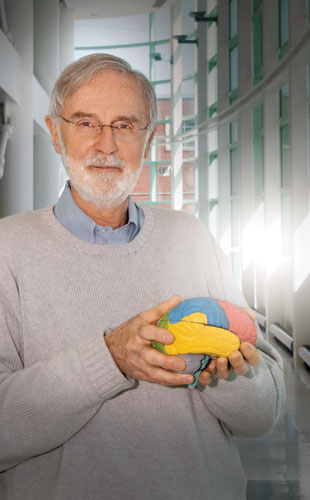
 MARCUS E. RAICHLE
MARCUS E. RAICHLE
Professor of Radiology, Neurology, Neurobiology and Biomedical Engineering Washington University School of Medicine, St. LouisWASHINGTON UNIVERSITYMarcus Raichle was a University of Washington junior majoring in history and political science when he took his first biology class to fulfill a science requirement. Introduction to zoology as taught by marine biologist Dixy Lee Ray was so transformative that he immediately switched his major to premed, says Raichle, who had to start his science education from scratch. After a year’s setback because of a misplaced invite for a medical school interview, Raichle was accepted at the University of Washington School of Medicine . “I felt like a fish out of water, surrounded by people who must have gotten out of the crib and said, ‘I want to go to medical school.’”
Raichle became fascinated by neuroscience. “I read our neuroanatomy textbook cover to cover, and I still have it,” he says. Raichle was particularly inspired by his teacher and subsequent mentor, Fred Plum, at that time the youngest person to chair a neurology department in the U.S. “He asked us in class what the relationship was between a pain and a tickling sensation, and I happened to know. Even though I was shy and not in the habit of raising my hand, I gave an answer that he appeared pleased with, and from that moment on, I felt like, ‘OK, I have arrived.’”
“I think, for better or worse, imaging has become the face of neuroscience.”
Since graduating from medical school in 1964, Raichle has been ...




















