Most people have a day where they don’t have as much energy as usual. They could have slept poorly or overexerted themselves the night or day before. However, individuals with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) experience severe chronic fatigue alongside pain, sleep disruptions, and difficulty focusing that profoundly affect their quality of life. In the US, the Centers for Disease Control and Prevention estimates that 3.3 million people have ME/CFS, but the condition has no known cause and no cure yet.
One of the reasons ME/CFS remains not well understood is because it is difficult to study. “We have no good biomarker,” said Carmen Scheibenbogen, a physician and immunologist at Charité University Medicine Berlin who studies ME/CFS. She added that while researchers see differences in various factors in some patients compared to healthy people, none of these distinguish ME/CFS as a whole. “Therefore, it’s most likely that we face subgroups of different patients.”
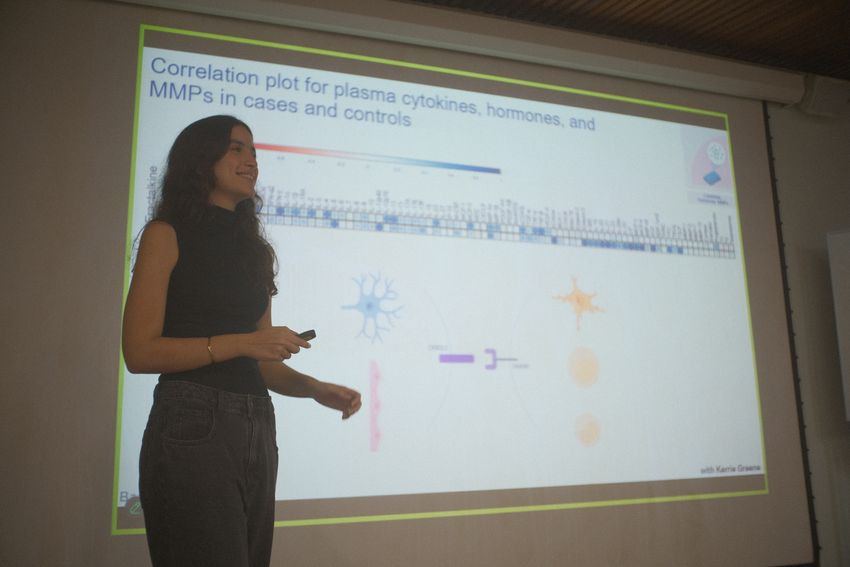
Victoria Bastos defended her PhD in June 2025, where she presented data from profiling subtypes of ME/CFS.
Pedro Miziara
This would be similar to other health maladies like diabetes mellitus and multiple sclerosis. “Perhaps the reason why we don't understand [ME/CFS] so well and the reason we don't have a biomarker is because we're looking at all the patients as having the same thing, and that in itself is masking us from finding a biomarker,” said Victoria Bastos, a physician-scientist at the Federal University of Rio de Janeiro.
Bastos previously studied variations of immune mechanisms in health and disease tolerance and resistance as a dual medical and graduate student in immunologist Marcelo Bozza’s group. During that time, she worked with patients who contracted SARS-CoV-2 and maintained long-term upper respiratory tract infections but resisted becoming severely ill. Inspired by the work of Akiko Iwasaki, an immunologist at Yale University who studies long COVID, Bastos joined Iwasaki’s group to profile immune markers in patients with ME/CFS. Along with collaborators at the Karolinska Institute and PolyBio Research Foundation, the team identified distinct clusters of ME/CFS patients based upon the presence of neuroinflammatory markers in the cerebrospinal fluid.1 The findings, published in The Journal of Immunology, offer new insights into ME/CFS pathology and potential avenues for more effective therapies.
The team first assessed circulating immune proteins, hormones, and matrix metalloproteinases (MMPs)—which have been associated in neuroinflammation—between people with ME/CFS and healthy participants.2,3 They only observed one cytokine, tumor necrosis factor-related apoptosis-inducing ligand (TRAIL), that was significantly increased in ME/CFS plasma compared to healthy controls. Studying potential interactions between these factors, the researchers showed that samples from ME/CFS had more positive correlations between the circulating factors than samples from controls. However, they identified strong positive correlation patterns from two cytokines involved in the central nervous system (CNS) and neuroinflammation in healthy controls that they did not see in samples from ME/CFS patients. Bastos said that this could be an area to further explore for differences in the proteins’ production and behavior between healthy and ME/CFS patients.
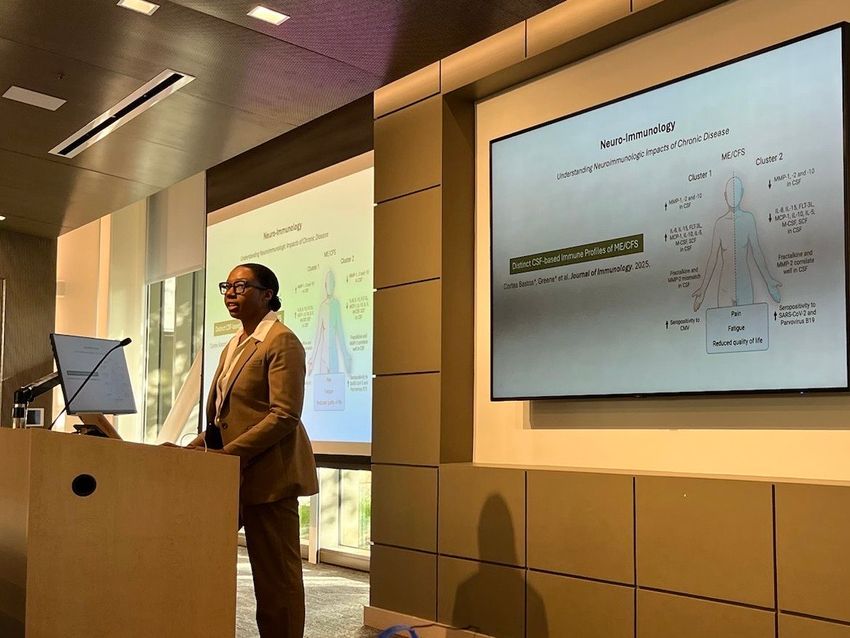
Kerri Greene, a graduate student in Akiko Iwasaki’s group at Yale University and study coauthor, presents her team’s data studying subtypes in ME/CFS.
Maria Isabel Barros Guinle
To study possible differences within ME/CFS patients, the team investigated the amount of MMPs in cerebrospinal fluid samples and observed a separation into two clusters based upon greater MMP content in one group. “I remember the second I first saw that graph, and I was like, ‘This is so, so amazing to be able to see it,’” said Bastos of the correlation data.
Next, the team studied 71 cytokines in the cerebrospinal fluid. They saw that eight of these factors differed between the two groups and that these cytokines were increased in the cluster with elevated MMP. Bastos said that this finding was also interesting. “We're really building this picture of a higher neuroinflammatory scenario in this cluster of the patients,” she said.
Scheibenbogen, who was not involved in the research, said that the study was well done and presented interesting findings, especially with the availability of cerebrospinal fluid. “It confirms that we indeed face subgroups. Also, regarding the immunological dysregulation, it tells us that we should look more into the CNS when we study these patients,” she said. She added that the differences in elevated neuroinflammatory markers could explain why some patients respond to drugs targeting this inflammation while others do not.
“I'm not saying we have definitively identified ME/CFS type 1 or 2, but what we hope that the work can show is that there is very strong evidence for this being a promising direction to go,” Bastos said, adding that the ability to subdivide patients could pave the way for individualized treatments.
- Bastos VC, et al. Cerebrospinal fluid immune phenotyping reveals distinct immunotypes of myalgic encephalomyelitis/chronic fatigue syndrome. J Immunol. 2025:vkaf087.
- Martino Adami PV, et al. Matrix metalloproteinase 10 is linked to the risk of progression to dementia of the Alzheimer’s type. Brain. 2022;145(7):2507-2517.
- Li Q, et al. MMP-2: A modulator of neuronal precursor activity and cognitive and motor behaviors. Behav Brain Res. 2017;333:74-82.
- de Almeida MMA, et al. Fractalkine enhances oligodendrocyte regeneration and remyelination in a demyelination mouse model. Stem Cell Rep. 2023;18(2):519-533.
- Huber AK, et al. An emerging role for eotaxins in neurodegenerative disease. Clin Immunol. 2018;189:29-33.














