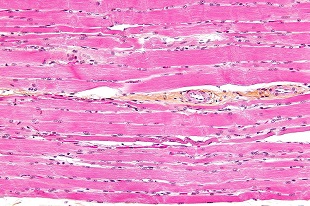
 WIKIMEDIA, NEPHRONResearchers have refined a method for regenerating large amounts of muscle lost after injury using material from pig bladders, according to a study published today (April 30) in Science Translational Medicine. A team from the University of Pittsburgh, led by Stephen Badylak, implanted extracelluar matrix, denuded of cells, from the lining of pig bladders, first into mice and eventually into five male patients.
WIKIMEDIA, NEPHRONResearchers have refined a method for regenerating large amounts of muscle lost after injury using material from pig bladders, according to a study published today (April 30) in Science Translational Medicine. A team from the University of Pittsburgh, led by Stephen Badylak, implanted extracelluar matrix, denuded of cells, from the lining of pig bladders, first into mice and eventually into five male patients.
“It’s a good correlation of a treatment of a muscle volumetric defect—in people—with an effort to understand the actual effect on muscle repair that’s occurring,” said Jason Pomerantz, who focuses on tissue regeneration at the University of California, San Francisco, but was not involved in the study.
The male patients all had traumatic muscle injuries—three from military incidents, two from skiing accidents—large enough to be classified as volumetric muscle loss. Muscle tissue is adept at repairing itself, but if a large enough chunk is lost, the remaining muscle cannot replenish what’s missing and usually fills in the gaps with scar tissue. Many researchers are investigating how to use stem cells or progenitor muscle cells to repair muscle injuries, but even the most successful to date ...



















