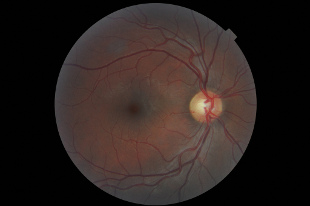
 FLICKR, SIMON LEEDelivering drugs to the posterior segment of the eye has long posed a challenge, due in large part to physiological barriers, which large, peptide-based molecules are unable to cross. Two recent studies highlight how innovative nanotechnology approaches are being used to overcome these roadblocks.
FLICKR, SIMON LEEDelivering drugs to the posterior segment of the eye has long posed a challenge, due in large part to physiological barriers, which large, peptide-based molecules are unable to cross. Two recent studies highlight how innovative nanotechnology approaches are being used to overcome these roadblocks.
Researchers led by Francesca Cordeiro, a professor of retinal neurodegeneration and glaucoma studies at University College London, used liposomes—lipid-based vesicles that can be loaded with drug molecules—to formulate eye drops for delivering Avastin, an anti-vascular endothelial growth factor (anti-VEGF) medication commonly used to treat age-related macular degeneration (AMD). The researchers proposed that liposome-based Avastin delivery is a promising alternative to the comparatively risky and invasive intraocular injections that are currently the only effective treatment for many AMD patients. Their work was published in Small this month (March 5).
Liposomes are well-established as drug-delivery systems, but getting them across ocular barriers has remained a challenge. Cordeiro’s group noticed that the lipid-binding protein Annexin A5 (AnxA5) was able to cross certain biological barriers, and was found in ...




















