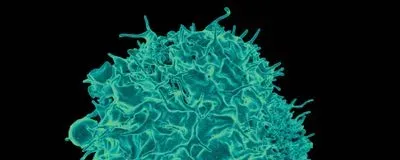
ABOVE: Vaccines against poxvirus and melanoma induced more memory T cells (shown) in mice when they entered through the lungs than when administered via another route.
FLICKR, NIAID
The paper
K. Rakhra et al., “Exploiting albumin as a mucosal vaccine chaperone for robust generation of lung-resident memory T cells,” Sci Immunol, 6:eabd8003, 2021.
Most vaccines are injected into muscle, where they induce systemic immunity. A goal of many vaccine developers is to engineer inhalable formulations that would build up powerful immunity localized in the mucous membranes that line organs such as the lungs. But to do so, vaccines need to breach that mucous membrane and head to the lymph nodes within the lungs, where they can instruct the immune system to generate memory T cells, key players in long-term immunity.
To accomplish that, Darrell Irvine, a biological engineer at MIT, and his team looked to albumin, a protein that naturally crosses mucous ...