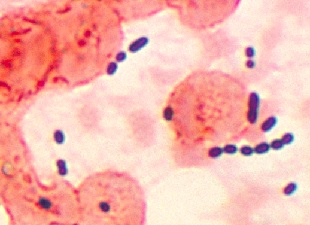
 Enterococcus in lung tissueWIKIMEDIA, CDC/MIKE MILLERGut microbes are known to play an important role in the body’s immune function. But antibiotics can deplete these bugs, leaving patients undergoing long-term treatment susceptible to infection by opportunistic, pathogenic bacteria, such as Vancomycin-resistant Enterococcus faecium (VRE). Building on mouse studies showing that murine norovirus can enhance intestinal immune system development, a team led by researchers at Memorial Sloan Kettering Cancer Center in New York City has now identified a norovirus-mimicking molecule that reduces VRE densities in antibiotic-treated mice. The findings were published today (February 24) in Science Translational Medicine.
Enterococcus in lung tissueWIKIMEDIA, CDC/MIKE MILLERGut microbes are known to play an important role in the body’s immune function. But antibiotics can deplete these bugs, leaving patients undergoing long-term treatment susceptible to infection by opportunistic, pathogenic bacteria, such as Vancomycin-resistant Enterococcus faecium (VRE). Building on mouse studies showing that murine norovirus can enhance intestinal immune system development, a team led by researchers at Memorial Sloan Kettering Cancer Center in New York City has now identified a norovirus-mimicking molecule that reduces VRE densities in antibiotic-treated mice. The findings were published today (February 24) in Science Translational Medicine.
“They showed not only that this [norovirus] is protective against VRE—which is a very serious, hospital-acquired pathogen—but that they could also mimic the effect of the virus using a drug,” said Kenneth Cadwell, an assistant professor of microbiology at New York University’s Skirball Institute of Biomolecular Medicine, who was not involved in the research. “That’s pretty amazing.”
The microbiota of the intestine normally provide indirect resistance to colonization by VRE and other pathogens by triggering the host immune system to produce antimicrobial proteins. But when the host community is depleted by antibiotics, VRE is free to proliferate, and can cause potentially life-threatening, difficult-to-treat infections.
Inspired by recent research in mice demonstrating that murine norovirus can enhance antibacterial defenses in the intestine, the team tested whether ...














