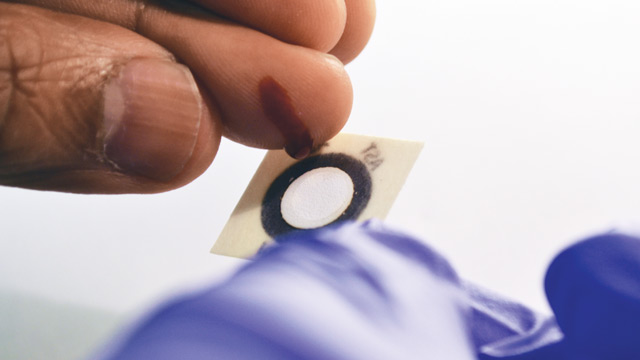
 JUST A DROP: This paper-based test, which costs less than $0.10, could help health care providers in developing countries monitor for liver toxicity associated with HIV and TB treatments.COURTESY OF DIAGNOSTICS FOR ALLHuman immunodeficiency virus (HIV) and tuberculosis (TB) are two of the leading killers in the world, taking an estimated 1.7 million and 1.4 million lives each year, respectively. The worldwide distribution of medications to treat these diseases has been a boon to global health, but some of those drugs can cause liver toxicity, so patients taking them need routine liver monitoring.
JUST A DROP: This paper-based test, which costs less than $0.10, could help health care providers in developing countries monitor for liver toxicity associated with HIV and TB treatments.COURTESY OF DIAGNOSTICS FOR ALLHuman immunodeficiency virus (HIV) and tuberculosis (TB) are two of the leading killers in the world, taking an estimated 1.7 million and 1.4 million lives each year, respectively. The worldwide distribution of medications to treat these diseases has been a boon to global health, but some of those drugs can cause liver toxicity, so patients taking them need routine liver monitoring.
In developed countries, that’s simply a matter of visiting the doctor’s office and having blood drawn. With a whiz in an electric centrifuge and a quick pass through an automated machine to detect liver metabolites, the results are in. But in developing countries such as Botswana and South Africa—areas plagued by HIV and TB infections—such tests are virtually nonexistent. And there are no alternatives. “In a resource-limited setting, monitoring isn’t happening at all,” says Nira Pollock, associate director of the Infectious Diseases Diagnostic Laboratory at Boston Children’s Hospital. In some cases, undetected liver damage can lead to organ failure and death.
Three years ago, Pollock joined forces with a local Massachusetts biotech company called Diagnostics For All (DFA) to develop a paper-based method for diagnosing ...















