Sleep disturbances are commonly reported by people with neurodegenerative conditions that damage motor neurons.1 Some of these disorders, including amyotrophic lateral sclerosis (ALS), affect nonmotor functions of the brain, including sleep, which is regulated by the hypothalamus.
This phenomenon captured the interest of Matei Bolborea, a neuroendocrinologist at the French National Institute of Health and Medical Research. Previous studies showing sleep disturbances in people with ALS looked exclusively at individuals in the late-stage of the disease, at which point respiratory symptoms are present, making it difficult to distinguish the effect of ALS degeneration on sleep.2,3 “What we wanted to know is, in fact, what happens before that?” Bolborea said.

Matei Bolborea and his team showed that ALS affects sleep even before symptoms begin.
Matei Bolborea
In a paper published in Science Translational Medicine, Bolborea and his team studied people with early-stage and presymptomatic ALS to gain insights into early changes to neurological functions.4 Additional studies using animal models of ALS shed light on the molecular underpinnings of the disease’s effects on sleep. Their findings suggest potential therapeutic strategies to improve quality of life and possibly symptom onset.
The researchers started by investigating differences in sleep quality between individuals who had early-stage ALS, a period before the onset of respiratory problems, and people without ALS or other motor deficits. They observed that people with ALS took longer to fall asleep and had increased bouts of wake and rapid eye movement (REM) sleep but reduced deep sleep non-REM (NREM) stages.
In a second cohort of individuals with an immediate relation to someone with ALS but who had not developed motor symptoms, the researchers recorded their sleep and collected DNA samples to determine which individuals carried a genetic mutation associated with ALS.
Compared to individuals with no ALS mutations, presymptomatic ALS carriers demonstrated altered sleep patterns that were dependent on the mutation that they carried: one mutation was associated with less overall time asleep and reduced deep sleep NREM, while a second mutation led to a longer time to fall asleep and more time in REM, but less time in total in NREM stages. Both mutations were associated with increased times in the wake period.
Although no participants indicated that they felt like they had interrupted sleep in either of the sleep studies, individuals with early-stage ALS and those presymptomatic for the condition performed worse on a test of cognitive functions.
The team confirmed the sleep changes they saw in their human studies using three different animal models of ALS with mutations in either an RNA-binding protein, a DNA-binding protein, or superoxide dismutase, all shown to be affected in the disorder. Although the onset of sleeping changes varied by genetic mutation, the researchers saw an overall decrease in NREM and REM and increased wake periods in animals; these changes occurred prior to motor deficits in one model. Thus, although the effects to REM sleep differed between mice and humans, ALS caused similar changes to sleep-wake patterns in both species.
Previously, the researchers observed that ALS causes degeneration in neurons that respond to melanin concentrating hormone (MCH).5 This neuropeptide, along with orexin, regulates sleep. Orexin is responsible for promoting wakefulness, while MCH sends people and animals into REM sleep.
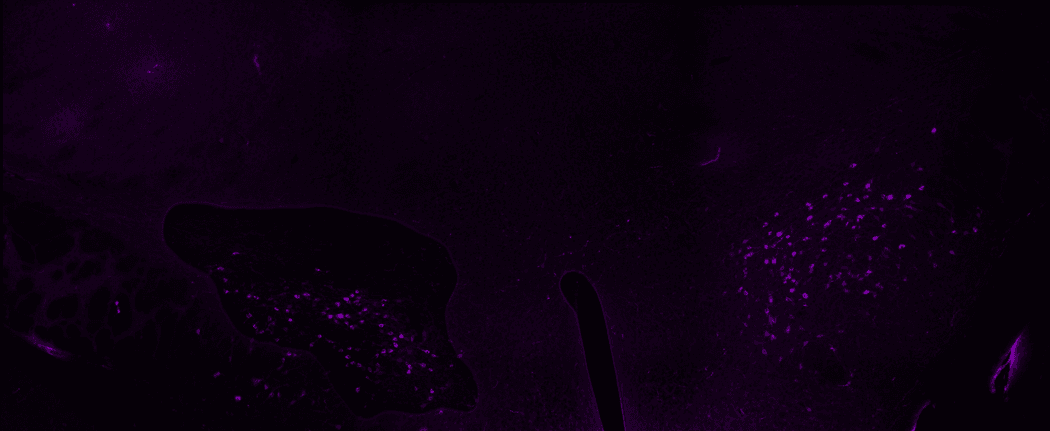
Bolborea’s team saw that blocking the neuropeptide orexin from binding its neurons (magenta clusters) improved the sleep patterns in mice with presymptomatic ALS.
Simon Guillot
To attempt to revert the ALS-induced sleep disruptions in the mice, they delivered MCH to the cerebral spinal fluid. In two models, MCH treatment decreased periods of wake and increased the time mice spent in REM sleep. Then, using a licensed orexin receptor antagonist, the team found that reducing this neuropeptide’s signaling improved sleep parameters across all their ALS models.
“What still needs to be worked out is what the neuroendocrine changes are and how we might target them in humans,” said Rebekah Ahmed, a neurologist at the University of Sydney who was not involved in the current study. In addition to sleep, orexin also regulates appetite. “If you affect orexin for sleep, how does that affect eating, metabolism, and the other functions of the hypothalamus as well?” Ahmed added.
“This is a very elegant and comprehensive, truly translational research study,” said Åsa Petersén, a neuroscientist at Lund University. Petersén was not involved in the present study but has collaborated with some of the coauthors on other projects studying the role of the hypothalamus in neurodegenerative disorders. “They show for the first time that there are changes in sleep before patients start to develop motor symptoms in ALS, and that's a very important finding,” Petersén added.
Bolborea said that studying sleep changes in individuals likely to develop ALS provides an opportunity to diagnose the disorder sooner. He and his team want to conduct a clinical trial to evaluate whether the orexin antagonist similarly restores sleep functions in humans. The team also plans to study mechanistically what occurs to these hypothalamic neurons in early ALS.
- Malhotra RK. Neurodegenerative disorders and sleep. Sleep Med Clin. 2022;17(2):307-314.
- Sun X, et al. Study on sleep-wake disorders in patients with genetic and non-genetic amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2020;92(1):96-102.
- Boentert M, et al. Effects of non-invasive ventilation on objective sleep and nocturnal respiration in patients with amyotrophic lateral sclerosis. J Neurol. 2015;262:2073-2082.
- Guillot SJ, et al. Early-onset sleep alterations found in patients with amyotrophic lateral sclerosis are ameliorated by orexin antagonist in mouse models. Sci Transl Med. 2025;17(783):eadm7580.
- Bolborea M, et al. Loss of hypothalamic MCH decreases food intake in amyotrophic lateral sclerosis. Acta Neuropathol. 2023;145(6):773-791.
















