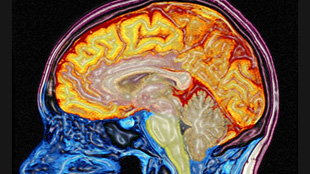
 WELLCOME IMAGES, MARK LYTHGOE & CHLOE HUTTON
WELLCOME IMAGES, MARK LYTHGOE & CHLOE HUTTON
By the time Alzheimer's is detectable, it's too late to change the course of the disease. But changes in protein levels may begin long before any signs of cognitive decline develop, according to a study published this month in the Archives of Neurology. The findings point to early markers that could be used to diagnose the disease before symptoms appear, potentially diverting damage before it’s irreversible.
“It is a fascinating study of differences in proteins by their functions in the cerebrospinal fluid,” Randall Bateman, a neurologist at Washington University in St. Louis, who was not involved in the study, told The Scientist in an e-mail. “The study demonstrates the power of proteomics in analyzing the complexities of human brain metabolism and points to new avenues ...




















