Despite the message many fitness influencers keep trying to push, fats are essential for the body to function properly. Too little and issues with hormone production, vitamin absorption, and nerve function might crop up. But too much fat isn’t good either. Decades of patient data unequivocally show that obesity increases the risk of hypertension, which subsequently raises the likelihood of developing cardiovascular diseases and strokes.1
But not all fat is the same. It’s the relative amounts of different types that’s key to blood pressure regulation, rather than the total fat level. Excess white fat, which the body uses to store calories, is associated with hypertension. Contrastingly, brown fat, which the body burns up to generate energy and heat, is linked to lower risk of high blood pressure.
“A couple of years ago, we conducted a large clinical study where we found that individuals that have brown fat had lower odds of having different cardiometabolic diseases, including type 2 diabetes and hypertension,” said Mascha Koenen, a molecular biologist at Rockefeller University, in a statement. “We had no mechanistic understanding why that would be the case.”
Paul Cohen and Mascha Koenen are molecular biologists at Rockefeller University who investigate the molecular origins of metabolic disease related to obesity.
Lori Chertoff for The Rockefeller University
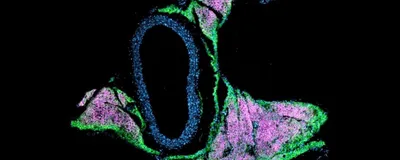
To gain a deeper understanding of this relationship, Koenen and her colleagues studied beige fat—the rodent equivalent of human brown fat—and its effect on vascular architecture and blood pressure in mice. Their findings, published in Science, showed that beige fat suppresses an enzyme that promotes stiffening of blood vessels and hypertension.2 These findings highlight brown fat as a new therapeutic target for high blood pressure and cardiovascular diseases.
“We started with a surprising and unexplained association and demonstrated a causal relationship and a biological mechanism,” said Paul Cohen, a physician and molecular biologist at Rockefeller University and coauthor of the study.
Human and rodent bodies have multiple heat-producing fat stores, some of which surround blood vessels to form the perivascular adipose tissue (PVAT). Cells in the PVAT secrete molecules that can cross the wall of the blood vessels and alter the architecture of the tissue within. Depending on the relative amounts of fat cell types in the PVAT, the molecules released can cause inflammation and constriction of the vessel walls. This made for an ideal model to study the relationship between beige fat and vascular health.
Next, the team created mutant mice that lacked beige fat production. These animals had higher levels of white fat markers in their PVAT, increased blood pressure, and stiff and fibrous tissue around their blood vessels as compared to their beige-fat-producing counterparts. When the researchers treated healthy vascular tissue with molecules secreted by fat cells lacking beige fat, they observed similar structural changes. Using single cell RNA-sequencing, Koenen and her colleagues identified quiescin sulfhydryl oxidase 1 (QSOX1) as the mediator of these changes, a tissue remodeling enzyme released by PVAT. In the absence of beige fat, levels of QSOX1 shot up, causing blood vessels to stiffen and constrict, which in turn caused the heart to work harder to pump blood. Mice lacking the Qsox1 gene did not have vascular dysfunction, even in the absence of beige fat.
“We've now confirmed that it's not just fat, per se, that contributes to hypertension, but the type of fat,” Cohen said.
Koenen and Cohen want to now move beyond mice and look for genetic determinants of brown fat function in humans. “The more we know about these molecular links, the more we can move towards conceiving of a world where we can recommend targeted therapies based on an individual’s medical and molecular characteristics,” Cohen said.
- Becher T, et al. Brown adipose tissue is associated with cardiometabolic health. Nat Med. 2021;27(1):58-65.
- Koenen M, et al. Ablation of prdm16 and beige fat identity causes vascular remodeling and elevated blood pressure. Science. 2026.