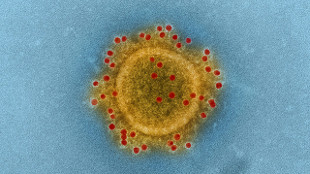
 FLICKR, NIAID
FLICKR, NIAID
South Korean officials today announced the end of the country’s recent Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak, but scientists studying the virus and others like it expect more outbreaks to follow.
“We think there will be other coronaviruses in the future that will be important and will need to be dealt with,” said Barney Graham, deputy director of the Vaccine Research Center at the National Institute of Allergy and Infectious Diseases (NIAID). In a paper published today (July 28) in Nature Communications, Graham and his colleagues described the antibody response to a vaccine candidate based on the MERS-CoV spike glycoprotein in mice, and characterized several murine virus-neutralizing monoclonal antibodies. The report follows on another study, published yesterday (July 27) in PNAS, in which researchers ...




















