 WIKIMEDIA, BRUCEBLAUSThe immune system is known for its ability to remember its response to pathogens, leading to more efficient clearance of the same pathogen upon reinfection. This immunological memory forms the basis of one of the most important medical achievements: infection prevention through vaccination.
WIKIMEDIA, BRUCEBLAUSThe immune system is known for its ability to remember its response to pathogens, leading to more efficient clearance of the same pathogen upon reinfection. This immunological memory forms the basis of one of the most important medical achievements: infection prevention through vaccination.
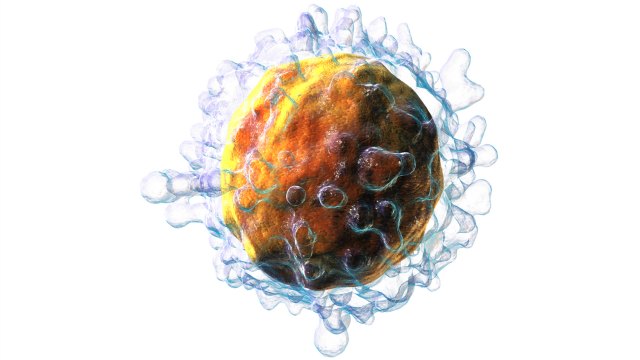
Any memory response to a pathogen, vaccine, or tumor starts with naive T cells. These cells are produced by the thymus and each have a unique T-cell receptor, recognizing a specific part of a pathogen. Critical for every T-cell response is the activation of T cells from their naive state. Only those naive T cells that recognize a pathogen via their T-cell receptors lose their naivety and differentiate into effector cells, which can kill infected cells or give help to other immune cells. Following pathogen clearance, most of the effector cells will die while a small pool of T cells develops into memory T cells, responsible for the quicker and stronger immune response upon a subsequent encounter of the pathogen.
Any memory response to a ...


















