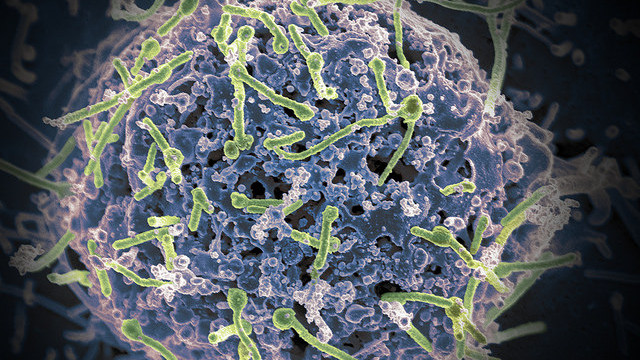
 FLICKR, NIAID
FLICKR, NIAID
Targeting just one region of an Ebolavirus protein with a monoclonal antibody can protect nonhuman primates from disease, according to a study of antibodies derived from an Ebola survivor’s immune cells. The results, published today (February 25) in Science, describe two Ebolavirus-neutralizing antibodies produced by a survivor of the 1995 outbreak in the Democratic Republic of Congo. One of the antibodies, whose unique binding properties are characterized in a companion paper also published today in Science, completely protected Rhesus macaque monkeys five days after infection with the virus.
“There’s been a lot of activity in the past year isolating monoclonal antibodies from human subjects,” said James Crowe, an immunologist at Vanderbilt University in Nashville who coauthored another recent study identifying antibodies from survivors of the ...


















