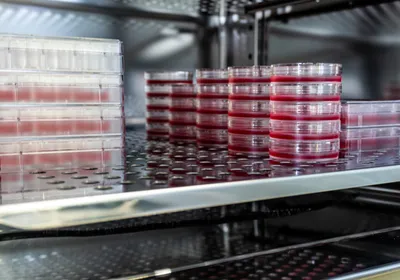
Human iPS cells differentiated into nerve cells (red). Credit: Bruce Conklin/Gladstone InstitutesJapanese scientists have produced skin and bone marrow from reprogrammed mouse stem cells, and transplanted these into genetically identical mice without triggering a strong immune reaction.
Human iPS cells differentiated into nerve cells (red). Credit: Bruce Conklin/Gladstone InstitutesJapanese scientists have produced skin and bone marrow from reprogrammed mouse stem cells, and transplanted these into genetically identical mice without triggering a strong immune reaction.
These results, published today (January 9) in Nature, should reassure researchers looking to use these cells—known as induced pluripotent stem cells (iPSCs)—to treat diseases. The future of such experimental therapies was thrown into question after a 2011 study, also published in Nature, found that iPSCs could face rejection by the immune system, even when injected into the same person who donated the cells. This immune response could destroy the transplants, rendering them ineffective as treatments.
Technical differences between the two contradicting studies make it difficult to assess whether iPSCs are truly safe from immune attacks. But Paul Knoepfler, a cell biologist from the University of California, Davis, who was not involved in either study, said that the new results were “very encouraging.” “[They] strongly suggest ...