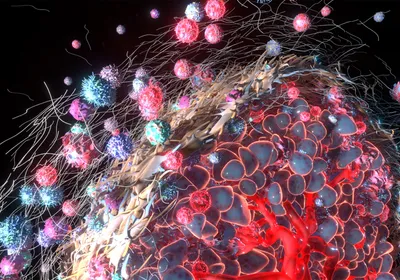
ABOVE: Certain types of immunotherapy treatment may cause latent infections of Mycobacterium tuberculosis to flare up in cancer patients, a new study warns.
© ISTOCK.COM, SELVANEGRA
In December 2012, an 80-year-old man in Florida went to his doctor to have a bulge on his eyelid examined. Tests showed that the bump was a rare form of skin cancer called Merkel cell carcinoma. Despite treatment, the man’s cancer spread, first to lymph nodes under his jaw, then to lymph nodes in his abdomen. So in June 2015, he enrolled in a clinical trial for Merck’s pembrolizumab (Keytruda), a checkpoint inhibitor drug that blocks programmed cell death protein 1 (PD-1) to help the immune system more effectively target and kill tumor cells.
Six months into receiving the experimental treatment, the man developed an odd-looking nodule in his lung that didn’t resemble any of his other tumors. Doctors decided to biopsy it. To their ...