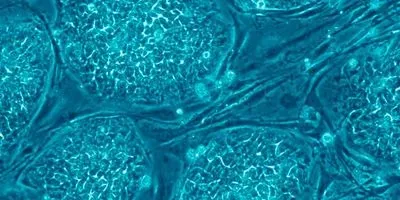
Human embryonic stem cellsWIKIMEDIA, NISSIM BEVENISTYDifferent cell culture conditions can impact genetic changes in human embryonic stem cells (ESCs), and these changes could affect the cells’ clinical utility, according to a study published in PLOS ONE today (February 25). Researchers from the Scripps Research Institute in La Jolla, California, and their colleagues have found that, overall, the fewest genetic changes arise in ESCs that are grown on a substrate layer of “feeder cells”—non-dividing cells that provide nutrients and help ESCs attach to their culture dishes—and passaged mechanically, that is, broken into clumps before being moved into new vessels. The researchers found that the most genetic variation arises in ESCs grown without feeder cells and passaged using an enzyme that dissociates them from a mass of tissue into single cells. Some of the observed genetic changes may even contribute to cancer, the researchers reported.
Human embryonic stem cellsWIKIMEDIA, NISSIM BEVENISTYDifferent cell culture conditions can impact genetic changes in human embryonic stem cells (ESCs), and these changes could affect the cells’ clinical utility, according to a study published in PLOS ONE today (February 25). Researchers from the Scripps Research Institute in La Jolla, California, and their colleagues have found that, overall, the fewest genetic changes arise in ESCs that are grown on a substrate layer of “feeder cells”—non-dividing cells that provide nutrients and help ESCs attach to their culture dishes—and passaged mechanically, that is, broken into clumps before being moved into new vessels. The researchers found that the most genetic variation arises in ESCs grown without feeder cells and passaged using an enzyme that dissociates them from a mass of tissue into single cells. Some of the observed genetic changes may even contribute to cancer, the researchers reported.
“The study is important in that it suggests that there are ways that we might avoid growing cells and having these abnormalities appear,” said stem-cell scientist Martin Pera of the University of Melbourne who was not involved in the work. “All of the changes would be a real concern, particularly for cells that are ultimately intended for therapeutic use.”
The take-home message, study coauthor Jeanne Loring of Scripps told The Scientist, is that researchers should monitor their cells. “This is like a mantra for me; it’s like a soap box. I’m trying to get other people in the field to closely examine their cells before they do anything else with them,” she said.
It’s long been known that ESCs undergo genetic changes in culture. It ...