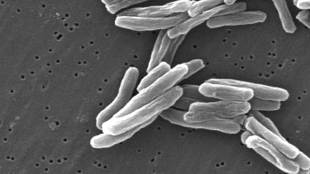
 Scanning electron micrograph of Mycobacterium tuberculosisWIKIMEDIA, CDC/JANICE CARRHigh doses of vitamin C can rapidly wipe out entire populations of drug-resistant strains of the bacteria that cause tuberculosis (TB) by inducing a chemical reaction that produces high levels of DNA-damaging oxidative radicals, according to a study published today (May 21) in Nature Communications.
Scanning electron micrograph of Mycobacterium tuberculosisWIKIMEDIA, CDC/JANICE CARRHigh doses of vitamin C can rapidly wipe out entire populations of drug-resistant strains of the bacteria that cause tuberculosis (TB) by inducing a chemical reaction that produces high levels of DNA-damaging oxidative radicals, according to a study published today (May 21) in Nature Communications.
The study was done on Mycobacterium tuberculosis in lab cultures, but if the results hold up in vivo, it raises the possibility that vitamin C could be added to existing TB drugs to speed up treatment. Moreover, by elucidating the mechanism by which vitamin C kills M. tuberculosis, the work suggests a promising route for the development of new TB drugs to tackle these hard-to-kill bacteria.
“[The research] shows that perhaps M. tuberculosis doesn’t have quite the iron-clad armor that we often associate with it; that is does perhaps have some Achilles heels and weak underbellies,” said William Bishai, director of the KwaZulu-Natal Research Institute for Tuberculosis and HIV in Durban, South Africa, who was not involved in the study.
But Bishai warned that it ...


















