In the early 2010s, three different groups, including a team at the National Cancer Institute (NCI), contemporaneously reported that chimeric antigen receptor (CAR) T cell therapy produced durable responses in patients with B cell cancers for the first time.1 Christopher Klebanoff, a cellular therapist and oncologist at Memorial Sloan Kettering Cancer Center, was doing a fellowship at the NCI when this watershed moment for the field of cell therapy occurred. These formative years in his training as a clinician scientist bolstered his interest in genetic engineering applications for studying T cell immunobiology.

Although the FDA has approved six CAR T cell therapies for liquid cancers, these therapies have struggled to make a breakthrough for solid tumors. One limitation of current CAR T cells is that they fail to discriminate between healthy and cancerous cells, depleting B cells in their wake. While clinicians can manage patients that lack circulating B cells, deploying the same widespread killing tactic is risky when treating cancers that mingle with organs. Additionally, the immunosuppressive tumor microenvironment, tumor heterogeneity, and antigen escape further limit CAR efficacy. Parallel to research exploring CAR system upgrades, some scientists have turned their attention to the potential of T cell receptor (TCR) therapies.2 Klebanoff, who studies adoptive T cell immunotherapies for treating solid cancers, discussed why the TCR is uniquely qualified to target tumor specific antigens, including neoantigens, and highlighted emerging cancer therapeutics that exploit TCR’s capacity to track and kill faulty cells.3
How can TCR-based therapeutics address the current limitations of treating solid tumors?
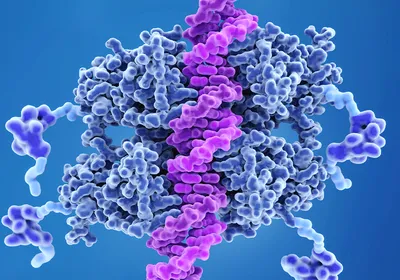
The TCR increases the number and types of proteins available to surveilling T cells. Unlike a CAR, which only detects antigens expressed on the surface of a cell, a TCR can also access the intracellular cancer proteome. This is the result of an elegant evolutionary process that equipped T cells with a sophisticated surveillance system: the human leukocyte antigen (HLA) presentation pathway. When the proteasome breaks down proteins inside a nucleated cell, including mutated proteins and those derived from pathogens, it produces short peptides. HLA molecules scoop these up and shuttle them to the cell’s surface for surveilling T cells to sample in search of foreign invaders.
A TCR can detect tiny amounts of these molecules; some researchers have found that as few as one to three peptides per cell can activate a TCR.4 For comparison, CAR T cells require thousands of copies of an antigen. As a result, even a subtle downregulation in the absolute amount of a target molecule, as seen with antigen escape, is enough to confer resistance to the therapy.
Diversity in the variable binding domains of the TCR’s alpha and beta chains facilitates detection of different HLA-peptide complexes. Scientists are taking a few different approaches to leverage the TCR’s elegant recognition system, including engineering the variable regions of the TCR and developing recombinant bispecific proteins that bind to specific HLA-peptide complexes.
What are the challenges in designing a TCR-based therapeutic?
The major bottleneck is finding targets that are uniquely and homogeneously expressed by cancer cells. Another challenge is that TCR therapeutics must be specific for the target antigen and also compatible with the HLA type of an individual. This is nontrivial because humans express diverse HLA types, which are akin to blood types, but rather than four different possibilities, there are tens of thousands of HLA molecules. Luckily, some HLA types are more common than others.5
This can complicate identifying patients who might benefit from a particular therapy because we need to confirm that the patient's cancer expresses the target antigen and that it is presented by a compatible HLA type. There will never be one TCR for all patients, but the goal is to create a library of vetted TCR that have the perfect mixture of potency, specificity, and compatibility so that we can accommodate as many patients as possible.
What makes a good TCR target?
The perfect intracellular TCR target is one that is homogeneously and uniquely expressed throughout the cancer cells and is shared among groups of patients. This avoids the need to develop expensive and bespoke one-off therapies. Additionally, it's a target that the cancer cell would find difficult to downregulate or lose if it's trying to escape detection from a targeted therapy. The focus of my lab is to search for these holy grail TCR targets.
A majority of tumor antigens are private neoantigens, or patient-specific targets that result from mutations that don’t affect cancer cell fitness and therefore are susceptible to antigen escape.6 Although a much smaller population, public neoantigens are shared by more than one patient and are essential for cancer cell survival, making them good targets for neoantigen-directed therapies.7 We’ve coalesced around peptides, or epitopes, that are derived from recurrent hotspot mutations in driver genes. Driver oncogenes are recurrently mutated genes—like Kirsten rat sarcoma virus (KRAS) and tumor protein p53—that drive cancer cell phenotypes, so a cancer cell would find it very difficult to lose expression of a driver gene and still grow, divide, and metastasize in an uncontrolled fashion.
We developed a strategy to look for recurrent driver mutations that are also bound and presented by common HLA types.7 By using this information, we can engineer a TCR to recognize these public neoantigens.
Why have TCR-based therapeutics taken so much longer than CAR therapies to enter oncology?
Using current technologies, it’s difficult to discover new TCR with a diverse binding profile or refine a TCR using current technologies. In contrast, monoclonal antibodies are the starting material for finding a binder for a CAR so the field really benefits from decades of research that streamlines the discovery of monoclonal antibodies that recognize specific targets, like phage display. Currently there isn’t a technology that similarly streamlines TCR discovery, but there are some really cool emerging technologies in the pipeline.
Thirty years ago, different groups of researchers came up with this brilliant idea that if they took a mouse and replaced its immunoglobulin locus—the genetic locus that makes antibodies—with the human sequence, they could generate humanized immunoglobulin mice that produced human antibodies.8 Since then, a couple of groups have used this same approach but for the TCR loci.9,10 The hope is that they can efficiently immunize the transgenic mouse against a specific human antigen in order to generate a diverse set of human TCR that are specific for that antigen.11
This interview has been edited for length and clarity.
- Levin AG, et al. CAR T cells: Building on the CD19 paradigm. Eur J Immunol. 2021;51(9):2151-2163.
- Klebanoff CA, et al. Prospects for gene-engineered T cell immunotherapy for solid cancers. Nat Med. 2016;22(1):26-36.
- Klebanoff CA, et al. T cell receptor therapeutics: Immunological targeting of the intracellular cancer proteome. Nat Rev Drug Discov. 2023;22:996-1017.
- Purbhoo MA, et al. T cell killing does not require the formation of a stable mature immunological synapse. Nat Immunol. 2004;5:524-530.
- Ellis JM, et al. Frequencies of HLA-A2 alleles in five US population groups: Predominance of A*02011 and identification of HLA-A*0231. Human Immunol. 2000;61(3):334-340.
- Parkhurst MR, et al. Unique neoantigens arise from somatic mutations in patients with gastrointestinal cancers. Cancer Discov. 2019;9(8):1022-1035.
- Chandran SS, et al. Immunogenicity and therapeutics targeting of a public neoantigen derived from mutated PIK3CA. Nat Med. 2022;28(5):946-957.
- Lonberg N. Human antibodies from transgenic animals. Nat Biotechnol. 2005;23(9):1117-1125.
- Moore MJ, et al. Humanization of T cell-mediated immunity in mice. Sci Immunol. 2021;6(66):eabj4026.
- Li LP, et al. Transgenic mice with a diverse human T cell antigen receptor repertoire. Nat Med. 2010;16(9):1029-1034.
- Obenaus M, et al. Identification of human T-cell receptors with optimal affinity to cancer antigens using antigen-negative humanized mice. Nat Biotechnol. 2015;33(4):402-407.