In 2024, a woman in China with type 1 diabetes (T1D) became the first person to have maintained independence from insulin for one year after receiving a transplantation of β cells derived from her own induced pluripotent stem cells (iPSCs).1 This accomplishment—a huge step forward in cell therapy for diabetes—was the fruit of two decades of labor by Hongkui Deng, a stem cell biologist at Peking University. He and several other researchers who contributed to the advances in stem cell biology and transplantation science are beginning to see their dream of cell therapies for diabetes management become a reality.
An Imperfect Solution to Controlling Sugar
In T1D, the immune system attacks insulin-producing cells, β cell islets, in the pancreas, resulting in a gradual decline in the availability of insulin to regulate blood sugar.2 Dysregulated blood sugar can cause overproduction of ketones, leading to increased blood acidity, and an array of cardiovascular complications.3 “The only therapy we can really provide right now in clinical practice to manage diabetes is to provide [patients] with insulin therapy,” explained Melena Bellin, a pediatric endocrinologist at the University of Minnesota.
While tools like insulin pumps and continuous glucose monitoring devices mitigate the risks of extreme events, according to Bellin, “Those systems still really don't replicate what the pancreatic islets do.”4,5
Although these and other advancements in diabetes detection and management have improved health outcomes for T1D patients, people with diabetes continue to experience reduced life expectancy, more health complications, and a decreased quality of life living with the risk of accidentally experiencing severe hypoglycemic episodes.6-8
These factors prompted research into better and more permanent treatments for T1D. The most obvious solution: restore the natural repertoire of β cell islets.
A Landmark in Cellular Opportunities

Hongkui Deng and his group demonstrated success in a new approach to developing stem cell-derived β cell islets and transplanting them into a novel site.
Xuexun Zhou
In 1990, Deng began his graduate studies at the University of California, Los Angeles, where he studied T cell responses and their involvement in T1D autoimmunity and the destruction of the β cell islets.9 That same year, scientists successfully transplanted β cell islets from cadavers into individuals with T1D, in which the first patient remained insulin-independent for up to 22 days after the procedure.10
Unfortunately, most patients who received cadaveric islet transplantations did not achieve full insulin independence, and many who did returned to requiring some amount of insulin within a year. Two problems emerged that were responsible for this poor success rate: difficulties in isolating sufficient numbers of islets and developing adequate immune suppression procedures that protected the graft from the immune system without damaging it.11 Advances in islet purification methods and an improved immune suppression approach in 2000 increased the post-transplantation success of insulin independence.12,13
Although most recipients experienced reduced instances of hypoglycemia, the majority returned to needing insulin within five years of the transplantation.14 Coupled with the limited supply of available cadaver pancreatic tissue, Deng and other scientists sought alternative options for diabetes cell therapy.
Toward the end of the 20th century, Deng turned his attention to the emerging field of stem cell biology. At that time, the monumental accomplishments of cloning with Dolly the Sheep and the successful culture of human embryonic stem cells (ESCs) gripped researchers like Deng with the possibilities for regenerative medicine.15 “Now I wanted to see if we can regenerate the β cell,” Deng said.
Many other scientists shared that enthusiasm; they began differentiating cultured ESCs into insulin-producing β cells.16 In 2006, stem cell biologists Shinya Yamanaka and Kazutoshi Takahashi, at Kyoto University at the time, demonstrated the ability to reprogram adult differentiated cells into a pluripotent state by modulating gene expression.17 These iPSCs overcame ethical limitations of ESCs and introduced the potential to use patients’ own cells in cell therapy, which could reduce the need for immune suppression in transplantations.18 Doug Melton’s group at Harvard University was the first to develop a protocol for producing stem-cell derived β cells at scale.19 This cell line is currently used by Vertex Pharmaceuticals in their trials for stem-cell derived therapies for diabetes.20
Whereas most researchers produced pluripotent cells following Yamanaka’s genetic approach, Deng, inspired by the regenerative abilities of animals like the axolotl and zebrafish, developed a method to reprogram cells through chemical biology.21
“Small molecules are more stable,” Deng said. “[They are] very easy for larger scale production and [they] also make chemical reprogramming processes standardized.”
Almost two decades after starting this project, Deng and his team demonstrated a successful method to revert differentiated human cells into a pluripotent state and then β cell islets using small molecules.22 The next step was determining where to place them in the body.
Location Matters in Cell Transplantation
Historically, physicians transplanted islets into the major vein of the liver. Although it is convenient and presents few surgical complications, this niche does not provide an ideal home for these cells.23,24 Even with immune suppression, innate immune cells attack the grafts.25 Additionally, although the ESC-derived cells rarely become tumorigenic, researchers showed that transplanted islets diffuse through the liver, making retrieval of the grafted cells in the event of a problem after transplantation complicated.26

Alice Tomei studies ways to improve cell therapy for diabetes through engineering immune cells.
Diabetes Research Institute Foundation
“You want to be able to make sure that there is no tumor formation at the site,” said Alice Tomei, an immunologist at The Diabetes Research Institute at the University of Miami. “Putting the cell throughout, in the bloodstream, in the liver, everywhere, it's not super, super ideal, especially if you move towards strategies for eliminating immunosuppression.”
To address these shortcomings, researchers explored other potential sites to introduce stem cell-derived β cell islets.27 Another group at Tomei’s institution pioneered transplantation into the omentum, a double-layered, fatty tissue that lines the abdominal cavity.28 “We call it [an] omental pouch,” Tomei said. “You make a little sandwich of islets in between two layers of omentum, and that stays in the [abdominal] cavity, stays localized.” In an initial Phase 1/2 clinical trial, this site demonstrated safety and some success in promoting the survival of transplanted β cell islets.29
Based on their preclinical studies exploring ideal transplantation locations, Deng’s team returned their reprogrammed β cell islets to their patient in a cavity between the subcutaneous fat and front abdominal muscle.30 In addition to this site promoting the survival and function of the islets, Deng said that this site allowed for easy removal of the transplanted cells if necessary, since they stayed contained in the cavity.
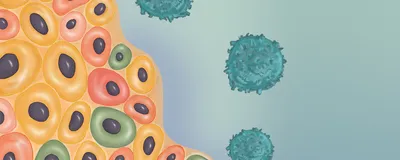
Advancing Stem Cell Therapy for Diabetes TreatmentOver the last two and a half decades, advancements in stem cell biology and immunology have improved the potential for cell therapy as a treatment for diabetes. Stem cells from different sources can be turned into the insulin-producing β cells lost in autoimmune attacks and returned to patients. While promising, lifelong immune suppression limits the ability to expand this option to patients. However, novel approaches may overcome this limitation.  modified from © istock.com, Rujirat Boonyong, ttsz, Olha Pohrebniak, Sakurra, metamorworks, Olga Kurbatova; designed by erin lemieux 1) Many clinical trials currently use validated human embryonic stem cell lines. Researchers differentiate these precursors into β cells, which form clusters, or islets (1a). Recently, some groups explored encapsulating these cells into a device to limit the access of immune cells to the transplanted islets (1b). Otherwise, the islets are transplanted directly into the patient, most often through the main liver vein (1c). 2) Recently, researchers successfully used a patient’s own cells for diabetes cell therapy. The team isolated adipose stem cells (2a) and induced these into pluripotent stem cells (2b) before differentiating them into β cell islets (2c). They transplanted these islets into a subcutaneous region in the abdomen (2d). 3) Because current cell therapy applications for diabetes require immune suppression, researchers are exploring approaches to protect β cells from the immune system to minimize lifelong modulation requirements. A few examples of preclinical approaches are as follows: encasing the islets into gel matrices which reduces contact with immune cells (3a); genetically engineering β cells to express immune suppressive proteins or deleting proteins to block immune attack (3b); delivering islets alongside immune modulatory cells, like mesenchymal stem cells (3c); and developing biomaterials or devices to provide localized immune regulatory molecules in the area of the transplants (3d). |
One year after this surgery, the patient remained insulin-independent and without any complications. “It's still remarkable in humans to see stem cell islets actually working that well in a site that is not the liver,” Tomei said.
However, she added that the long-term efficacy of the cells in this site remains to be seen, in particular because of the problem that many β cell transplantations face: autoimmune reawakening. Even with immune suppression, some patients experience a recurrence of the immune attack characteristic of diabetes, leading to destruction of the new cells.31
Finding Alternatives to Immune Suppression in Diabetes Cell Therapy
Another challenge in diabetes cell therapy is the lifelong need for immune suppression. In the case of non-self-cells, this is twofold, since the transplanted β cells would be seen as foreign to the immune system, and then the autoimmune components would be at play.
“From a broader picture, the induced pluripotent stem cells have a lot of appeal in terms of some of those immunosuppression questions,” said Bellin. However, she continued, “Manufacturing basically an individual drug for every single patient, that's potentially a real challenge in terms of clinical application, whereas the embryonic stem cell lines, you can use one manufacturing process to treat everyone.”
Tomei agreed, adding that until Deng’s study, all cell therapies that have gone to clinical trials have been conducted with cell lines, which furthers the need for immune suppression to prevent the transplants from being rejected.
In Deng’s patient iPSC-derived β cell islets therapy trial, the patient was already on immune suppressing drugs, so the researchers were not able to evaluate how well patient-derived cells compared to non-self-cells in terms of graft survival. However, considering that this patient and others still have T1D, with the current method, recipients would likely require some immune suppression to prevent their reprogrammed cells from being attacked by their autoimmune response. “We need to find the cell that can escape the autoimmune response attack, so the patient doesn't need to take the immunosuppression drugs. That's our next goal,” Deng said.
The problem of autoimmunity and immune suppression remains a problem in making cell therapy more realistic as a diabetes intervention. Long-term immune suppression presents risks for patients; additionally, many of these current pharmaceuticals are also toxic to the transplanted cells themselves.32,33
To address these issues and reduce the need for immune suppression altogether, researchers turned to techniques to protect cells against the immune system. In 2018, ViaCyte, a biotechnology company that explored stem cell-derived therapies for T1D and was later acquired by Vertex Pharmaceuticals, trialed one such encapsulating device.34 It was comprised of a polyester mesh and polymer membranes that separated the stem cell-derived β cells from the immune system, reducing the chance for immune cells to interfere with the transplanted cells and gives researchers the ability to remove the cells if that need arises.
However, it also minimized the amount of oxygen and other nutrients that the transplanted cells receive, which chokes the transplanted cells.35 To allow for necessary vascularization and gas exchange, ViaCyte developed a perforated device.36,37 Although this improved β cell survival and improved blood sugar control in a subset of patients, none became insulin-independent and the trial participants needed immune suppression therapy.
“That's been really, really challenging, because if you don't allow blood supply to get to those cells—β cells are highly oxygenated in the native pancreas and depend on good oxygen delivery—it's not clear that you get enough cell survival yet to be able to really have a meaningful clinical benefit, or at least no one has been able to demonstrate that yet, with the fully encapsulated product,” said Bellin said, who performed the transplantation surgeries at one of the sites of ViaCyte’s clinical trial. She also sits on the data safety monitoring board for Vertex Pharmaceuticals.

Coating β cell islets in a biocompatible matrix could protect them from immune destruction. Tomei’s lab licensed this technology to Sernova, a biotechnology company.
Aaron Stock and Grisell Gonzalez
As an alternative to macroencapsulation, other researchers developed microencapsulation approaches, such as coating β cells in a matrix that prevents physical interaction with immune cells but promotes nutrient and gas exchange.38 While initial cell coating approaches resulted in clusters that prevented proper diffusion, Tomei’s group has improved upon this method.39,40 “We wrap these materials around the cells, so we make it as small as possible,” Tomei said.
As opposed to separating transplanted cells from the immune system, other researchers seek to hide incoming β cells from the patient’s defense cells altogether.
In one example, researchers took the concept of an immune suppressive environment from tumors and applied it to the islet grafts. A biomaterial expressing immune suppressive programmed cell death-ligand 1 (PD-L1) transplanted alongside pancreatic islets reduced local immune activation and preserved the transplanted cells in animals.41 “They tell the cells to calm down,” Tomei said.
Another approach reimagines drug delivery.42 “What people have been doing, including in my lab, is to try to put these drugs only where they’re needed,” Tomei said. Her group used drug-associated nanomaterials to target and localize to sites of inflammation, such as a graft site.43
Scientists are also attempting to genetically engineer cells prior to transplantation to protect them from the immune system. Some preclinical approaches enhanced the expression of immune regulatory proteins, including PD-L1, on the β cells.44,45 “There is other work ongoing that shows that delivering cells, for example, stem cell-like mesenchymal stem cells, that are also modified to secret or present factors that can also act as bodyguards,” Tomei said.46
Alternatively, some researchers aim to engineer the transplanted cells themselves to protect them from immune attack. One group eliminated a key cellular identification protein that immune cells use to recognize and attack non-self-cells in stem cells.47 “They are trying to make these cells invisible to the immune system, and the way that you do that is by deleting their fingerprints,” Tomei said. She added that this could potentially also reduce autoimmune attacks, since these identification proteins are how the immune system instigates these responses.
Instead of modulating the immune system recognition in these cells, which raises concerns about surveillance against cancerous cells, another group identified a gene associated with T1D autoimmunity and deleted this gene.48 This protected transplanted β cells in a mouse model.
Changing Lives, One Cell at a Time
At this time, because of the limited long-term success in cell therapy and immune suppression it involves, stem-cell derived β cell transplantation is not a general treatment for diabetes. Even in clinical trials, only individuals who experience severe episodes of hypoglycemia are typically enrolled. However, this potential treatment already has a lot of interest amongst patients.
“There are individuals who, even without complicated diabetes, would be interested in potentially taking the risks of immunosuppression, just to have that freedom, that daily freedom from the intensive diabetes management—the potential to get off insulin,” Bellin said. Other patients, while eager for a more permanent resolution to diabetes, are content to wait until immune suppression is not necessary to the extent that it currently is.
Even with current challenges to overcome immune suppression: “The stem-cell derived islets, I think, are really a huge, huge step forward,” Bellin said.
“I'm really excited, because I've never seen that much progress being done that quickly, and so much interest. So it's really beautiful what is happening, and it's also nice how people are disclosing things, and so we know what the progress is,” Tomei said.
Already, in the cases where cell therapy leads to glucose control and insulin independence, it makes a huge impact on people’s lives. By providing long-term insulin independence, this intervention reduces the stress of experiencing low blood sugar events. However, this freedom also improves the mundane aspects of people’s lives. Deng cited the experience of the first patient in their self-iPSC-derived β cell islet study. Before her treatment, she ate only non-sugar varieties of products for the previous 11 years. Post treatment, he recalled how she was overjoyed to experience the difference in taste between foods like yogurt and ice cream that had real sugar. “She can eat anything she likes,” he said.
- Wang S, et al. Transplantation of chemically induced pluripotent stem-cell-derived islets under abdominal anterior rectus sheath in a type 1 diabetes patient. Cell. 2024;187(22):6152-6164.e18.
- Chen C, et al. Human beta cell mass and function in diabetes: Recent advances in knowledge and technologies to understand disease pathogenesis. Mol Metab. 2017;6(9):943-957.
- Longendyke R, et al. Acute and chronic adverse outcomes of type 1 diabetes. Endocrin Metab Clin N Am. 2024;53(1):123-133.
- Turksoy K, et al. Automated insulin delivery—The light at the end of the tunnel. J Pediatr. 2017;186:17-28.e9.
- Dovc K, Battelino T. Evolution of diabetes technology. Endocrin Metabol Clin. 2020;49(1):1-18.
- Miller RG, et al. Improvements in the life expectancy of type 1 diabetes: The Pittsburgh epidemiology of diabetes complications study cohort. Diabetes. 2012;62(11):2987-2992.
- Gregory GA, et al. Global incidence, prevalence, and mortality of type 1 diabetes in 2021 with projection to 2040: A modelling study. Lancet Diabetes Endocrinol. 2022;10(10):741-760.
- Talbo MK, et al. Effect of diabetes technologies on the fear of hypoglycaemia among people living with type 1 diabetes: A systematic review and meta-analysis. eClinicalMedicine. 2023;62:102119.
- Deng H, et al. Determinant capture as a possible mechanism of protection afforded by major histocompatibility complex class II molecules in autoimmune disease. J Exp Med. 1993;178(5):1675-1680.
- Scharp DW, et al. Insulin independence after islet transplantation into type I diabetic patient. Diabetes. 1990;39(4):515-518.
- Zeng Y, et al. The effect of prednisone on pancreatic islet autografts in dogs. Surgery. 1993;113(1):98-102.
- Lakey JRT, et al. Intraductal collagenase delivery into the human pancreas using syringe loading or controlled perfusion. Cell Transplant. 1999;8(3):285-292.
- Shapiro AMJ, et al. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Eng J Med. 2000;343(4):230-238.
- Ryan EA, et al. Five-year follow-up after clinical islet transplantation. Diabetes. 2005;54(7):2060-2069.
- Thomson JA, et al. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282(5391):1145-1147.
- Assady S, et al. Insulin production by human embryonic stem cells. Diabetes. 2001;50(8):1691-1697.
- Takahasi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126(4):663-676.
- Tateishi K, et al. Generation of insulin-secreting islet-like clusters from human skin fibroblasts. J Biol Chem. 2008;283(46):31601-31607.
- Pagliuca FW, et al. Generation of functional human pancreatic β cells in vitro. Cell. 2014;159(2):428-439.
- Reichman TW, et al. Glucose-dependent insulin production and insulin-independence in type 1 diabetes from stem cell-derived, fully differentiated islet cells—updated data from the VX-880 clinical trial. Diabetes. 2023;72(Supplement_1):836-P.
- Hou P, et al. Pluripotent stem cells induced from mouse somatic cells by small-molecule compounds. Science. 2013;341(6146):651-654.
- Du Y, et al. Human pluripotent stem-cell-derived islets ameliorate diabetes in non-human primates. Nat Med. 2022;28(2):272-282.
- Kawahara T, et al. Portal vein thrombosis is a potentially preventable complication in clinical islet transplantation. Am J Transplant. 2011;11(12):2700-2707.
- Shapiro AMJ, et al. Islet cell transplantation. Lancet. 2021;358:S21.
- Kanak MA, et al. Inflammatory response in islet transplantation. Int J Endocrinol. 2014;1:451035.
- Eriksson O, et al. Positron emission tomography in clinical islet transplantation. Am J Transpl. 2009;9(12):2816-2824.
- Cantarelli E, Peimonti L. Alternative transplantation sites for pancreatic islet grafts. Curr Diab Rep. 2011;11:364-374.
- Berman DM, et al. Bioengineering the endocrine pancreas: Intraomental islet transplantation within a biologic resorbable scaffold. Diabetes. 2016;65(5):1350-1361.
- Baidal D, et al. Long-term function of islet allografts transplanted on the omentum using a biological scaffold. Diabetes. 2018;67(Supplement_1):140-OR.
- Liang Z, et al. Implantation underneath the abdominal anterior rectus sheath enables effective and functional engraftment of stem-cell-derived islets. Nat Metabol. 2023;5(1):29-40.
- Vendrame F, et al. Risk factors for type 1 diabetes recurrence in immunosuppressed recipients of simultaneous pancreas-kidney transplants. Am J Transpl. 2016;16(1):235-245.
- Rostambeigi N, et al. Unique cellular and mitochondrial defects mediate FK506-induced islet β-cell dysfunction. Transplantation. 2011;91(6):615-623.
- Nir T, et al. Recovery from diabetes in mice by β cell regeneration. J Clin Invest. 2007;117(9):2553-2561.
- Henry RR, et al. Initial clinical evaluation of VC-01TM combination product—A stem cell-derived islet replacement for type 1 diabetes. Diabetes. 2018;67(Supplement_1):138-OR.
- Komatsu H, et al. Oxygen environment and islet size are the primary limiting factors of isolated pancreatic islet survival. PLoS ONE. 2017;12(8):e0183780.
- Keymeulen B, et al. Encapsulated stem cell–derived β cells exert glucose control in patients with type 1 diabetes. Nat Biotechnol. 2024;42:1507-1514.
- Shapiro AMJ, et al. Insulin expression and C-peptide in type 1 diabetes subjects implanted with stem cell-derived pancreatic endoderm cells in an encapsulation device. Cell Rep Med. 2021;2(12):100466.
- Tomei AA, et al. Device design and materials optimization of conformal coating for islets of Langerhans. Proc Natl Acad Sci USA. 2014;111(29):10514-10519.
- Touch BE, et al. Safety and viability of microencapsulated human islets transplanted into diabetic humans. Diabetes Care. 2009;32(10):1887-1889.
- Williams SJ, et al. Reduction of diffusion barriers in isolated rat islets improves survival, but not insulin secretion or transplantation outcome. Organogenesis. 2010;6(2):115-124.
- Coronel MM, et al. Immunotherapy via PD-L1–presenting biomaterials leads to long-term islet graft survival. Sci Adv. 2020;6(35):eaba5573.
- Paez-Mayorga J, et al. Neovascularized implantable cell homing encapsulation platform with tunable local immunosuppressant delivery for allogeneic cell transplantation. Biomaterials. 2020;257:120232.
- De Toni T, et al. Drug integrating amphiphilic nan-assemblies: 2. Spatiotemporal distribution within inflammation sites. Pharmaceutics. 2024;16(5):652.
- El Khatib MM, et al. β-Cell-targeted blockage of PD1 and CTLA4 pathways prevents development of autoimmune diabetes and acute allogeneic islets rejection. Gene Ther. 2015;22(5):430-438.
- Yoshihara E, et al. Immune-evasive human islet-like organoids ameliorate diabetes. Nature. 2020;586(7830):606-611.
- Wu H, et al. Genetically modified mesenchymal stem cells for improved islet transplantation. Mol Pharm. 2011;8(5):1458-1470.
- Gornalusse GG, et al. HLA-E-expressing pluripotent stem cells escape allogeneic responses and lysis by NK cells. Nat Biotechnol. 2017;35(8):765-772.
- Cai EP, et al. Genome-scale in vivo CRISPR screen identifies RNLS as a target for beta cell protection in type 1 diabetes. 2020;2(9):934-945.