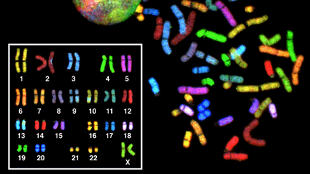
 WIKIMEDIA, NATIONAL HUMAN GENOME RESEARCH INSTITUTEInduced pluripotent stem cells (iPSCs) grown from the skin cells of a person with Down syndrome are helping researchers grow cerebral organoids and track protein expression in an effort to better understand the disorder on a cellular and molecular level. University of Colorado Boulder postdoc Tristan McClure-Begley and his colleagues sought to better understand the neurological and developmental changes that occur in people with a third copy of chromosome 21, the unifying pathological feature of Down syndrome. “That third copy of chromosome 21 influences all aspects of embryonic development, including critical steps during brain development,” McClure-Begley said in a statement. “But we’ve had trouble identifying exactly why the extra chromosome has such widespread effects, partly because we’ve lacked good human tissue models of Down syndrome.”
WIKIMEDIA, NATIONAL HUMAN GENOME RESEARCH INSTITUTEInduced pluripotent stem cells (iPSCs) grown from the skin cells of a person with Down syndrome are helping researchers grow cerebral organoids and track protein expression in an effort to better understand the disorder on a cellular and molecular level. University of Colorado Boulder postdoc Tristan McClure-Begley and his colleagues sought to better understand the neurological and developmental changes that occur in people with a third copy of chromosome 21, the unifying pathological feature of Down syndrome. “That third copy of chromosome 21 influences all aspects of embryonic development, including critical steps during brain development,” McClure-Begley said in a statement. “But we’ve had trouble identifying exactly why the extra chromosome has such widespread effects, partly because we’ve lacked good human tissue models of Down syndrome.”
So McClure-Begley and his colleagues took a fibroblast from a single Down syndrome patient, coaxed it into becoming two iPSC lines, and then reprogrammed those cells into neural progenitor cells that self-organized into cerebral tissue in vitro. “So we get a window into what an individual central nervous system development looked like from a cellular and molecular level,” he said during a Monday (October 19) press conference at the Society for Neuroscience (SfN) annual meeting held in Chicago.
The researchers found that protein expression did not follow a simple 1:1 ratio with the extra genes on the triplicate chromosome 21 leading to a proportional increase in proteins expressed. “Rather, there’s a complex change, where some proteins are upregulated, some proteins are downregulated—all reflecting a general ...




















