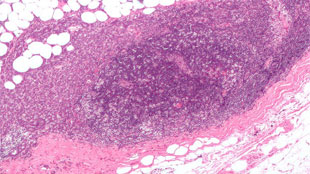
 Breast cancer cells invading a lymph nodeWIKIMEDIA COMMONS, NEPHRON
Breast cancer cells invading a lymph nodeWIKIMEDIA COMMONS, NEPHRON
When people die from breast cancer, it is mostly because their original tumours have metastasized to other organs. However, clinical trials for cancer drugs are focused on shrinking existing tumors, not preventing cancer spread. According to Patricia Steeg from the National Cancer Institute, this emphasis is stifling the discovery of chemicals that could prevent metastasis—costing money and patient lives.
In a comment piece, published today in Nature, Steeg calls on the US Food and Drug Administration (FDA) to usher in a new type of randomized clinical trial that will demonstrate if drugs could stop breast cancer from spreading.
Animal studies have identified several compounds could potentially prevent metastasis, but these chemicals often do not kill cancer cells or tumors that have already spread. When they ...