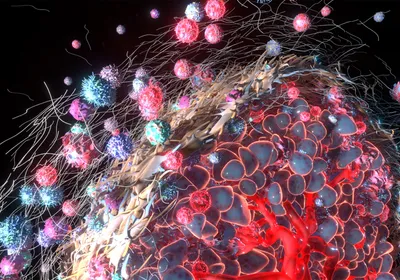
WIKIMEDIA, TOM MALLINSONDelivering DNA that results in the production of a tumor cell-specific reporter protein detectable in the blood could be a new method for earlier tumor identification, according to a proof-of-concept study published today (February 23) in PNAS.
WIKIMEDIA, TOM MALLINSONDelivering DNA that results in the production of a tumor cell-specific reporter protein detectable in the blood could be a new method for earlier tumor identification, according to a proof-of-concept study published today (February 23) in PNAS.
“Conceptually, this is transformative. There are many studies that put . . . gene-delivery systems into cancer cells and try to kill the cancer cells,” said Shuk-Mei Ho of the University of Cincinnati, who was not involved in the study. “[Instead] we might be able to do a lot of things to kill the cancer cells, including radiation or surgery, if we detect them early enough.”
Tumor cells generally release so few cancer-specific biomarker molecules into the bloodstream that these markers cannot be reliably used early disease detection. To circumvent this problem, Sanjiv “Sam” Gambhir and his colleagues at Stanford University designed injectable tumor-detecting DNA “minicircles.” Minicircles are similar to but smaller than bacterial plasmids and lack prokaryotic features such as antibiotic-resistance genes, thus minimizing ...