 LEAF BIO/MAPP BIOPHARMACEUTICALCan a piece of film half the size of a standard Band-Aid protect women from HIV and genital herpes? That’s the promise of MB66, a “multipurpose prevention technology” being developed by San Diego–based firm Leaf Bio, an arm of the company that developed the experimental Ebola treatment ZMapp last year.
LEAF BIO/MAPP BIOPHARMACEUTICALCan a piece of film half the size of a standard Band-Aid protect women from HIV and genital herpes? That’s the promise of MB66, a “multipurpose prevention technology” being developed by San Diego–based firm Leaf Bio, an arm of the company that developed the experimental Ebola treatment ZMapp last year.
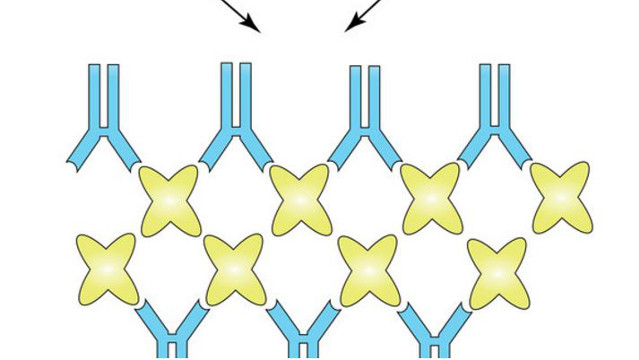
MB66 is a quick-dissolving film that carries antiviral human monoclonal antibodies—grown in plants—to the mucosal surface of the vagina. In preclinical tests, the film has worked to block viral transmission for periods of 12 to 24 hours.
In an upcoming clinical trial, immunologist Deborah Anderson of Boston University and her collaborators will test the safety of MB66 in a small cohort of women. If this prototype is successful, the strategy of delivering topical antibodies via the film could be expanded to include antibodies against other sexually transmitted infections, or even against sperm, to act as a contraceptive. “Localized antibodies may be more effective than intravenous because we’ll be able to introduce a higher concentration of the antibodies where they’re needed, so we think this approach ...



















