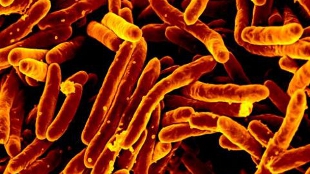
 WIKIMEDIA, NIAIDMycobacterium tuberculosis (TB) hides out in stem cells deep within bone tissue, where it avoids detection from the immune system and drugs, according to a study published last week (January 30) in Science Translational Medicine.
WIKIMEDIA, NIAIDMycobacterium tuberculosis (TB) hides out in stem cells deep within bone tissue, where it avoids detection from the immune system and drugs, according to a study published last week (January 30) in Science Translational Medicine.
“This is a very exciting story,” said Horacio Frydman, a microbiologist at Boston University who was not involved in the research. In 2006, Frydman and his Princeton University postdoc advisor, Nobel Laureate Eric Wieschaus, reported the first case of bacteria living in a stem cell niche, after observing Wolbachia invade the stem cells of the Drosophila melanogaster germline. "Hitching a ride in cells that are self-renewing is a great strategy for reinfecting tissues in the host”, continued Frydman, “and we always assumed that other bacteria should also be doing the same.”
Ninety percent of TB infections are cleared by the body’s immune defenses or by taking anti-TB medication. In the remaining 10 percent of cases, however, TB persists as a dormant, non-replicating infection. Though latent ...





















