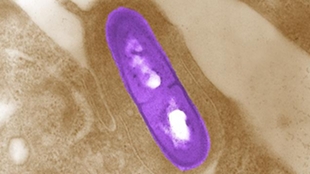
 Listeria monocytogenesCDC/ Dr. BALASUBR SWAMINATHAN; PEGGY HAYESA weakened strain of bacteria can deliver radiation to mouse pancreatic tumors while leaving normal tissue unscathed, according to new research published today (April 22) in Proceedings of the National Academy of Sciences. Researchers found that treating mice with radioactively labeled, attenuated Listeria monocytogenes drastically reduced the number of metastases, suggesting that the strategy holds promise as a targeted anti-cancer therapy with limited side effects.
Listeria monocytogenesCDC/ Dr. BALASUBR SWAMINATHAN; PEGGY HAYESA weakened strain of bacteria can deliver radiation to mouse pancreatic tumors while leaving normal tissue unscathed, according to new research published today (April 22) in Proceedings of the National Academy of Sciences. Researchers found that treating mice with radioactively labeled, attenuated Listeria monocytogenes drastically reduced the number of metastases, suggesting that the strategy holds promise as a targeted anti-cancer therapy with limited side effects.
The notion of using bacteria to attack tumors—often by helping to elicit an anti-cancer immune response or delivering a chemotherapeutic agent to cancer cells—is not new, noted Robert Hoffman, a cancer biologist at the University of California, San Diego, who was not involved in the current study. Hoffman’s own research on engineered Salmonella has shown that the bacteria can kill mouse cancer cells, including metastases of pancreatic cancer. And a Listeria strain called CRS-207 that expresses a tumor-associated protein has demonstrated safety and the ability to stimulate an immune response in Phase 1 and 2 trials of cancer patients. But in the new study, researchers at Albert Einstein College of Medicine in New York have paired this technique with a radioactive isotope to selectively kill ...



















