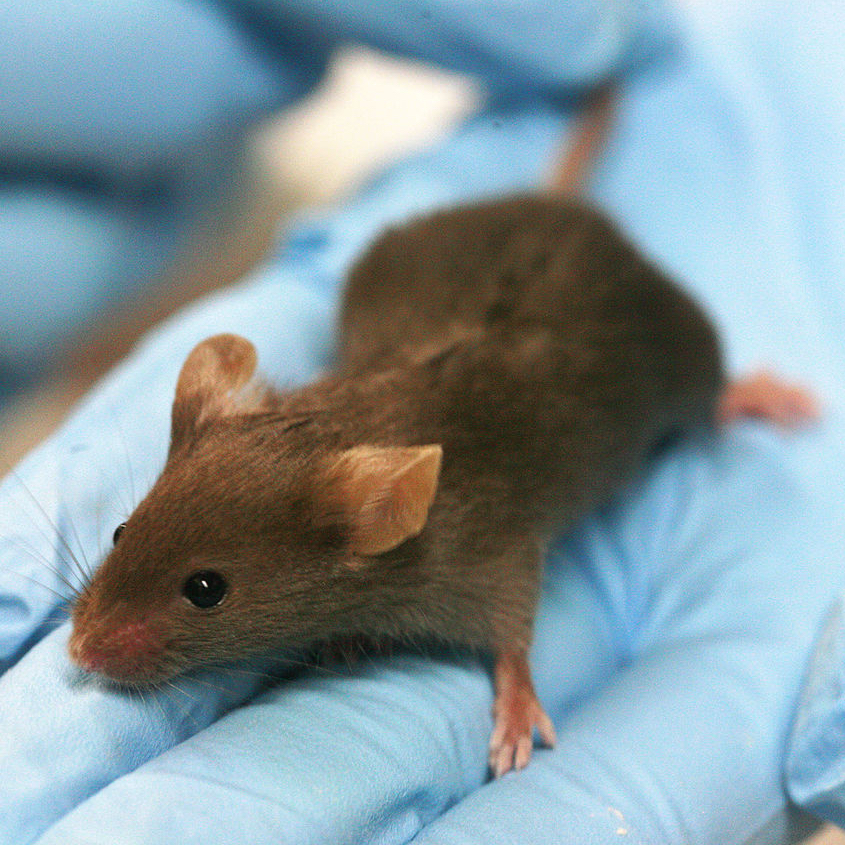
 WIKIMEDIA, RAMAGenetic variation underlies most cases of type 1 diabetes. According to a mouse study published today (August 22) in Nature Microbiology, perturbations to the gut microbiome may also play an important role. Mice genetically predisposed to type 1 diabetes that received antibiotics during infancy ran a higher risk of developing the disease, researchers from New York University and their colleagues have shown.
WIKIMEDIA, RAMAGenetic variation underlies most cases of type 1 diabetes. According to a mouse study published today (August 22) in Nature Microbiology, perturbations to the gut microbiome may also play an important role. Mice genetically predisposed to type 1 diabetes that received antibiotics during infancy ran a higher risk of developing the disease, researchers from New York University and their colleagues have shown.
“I find it to be a fantastic observation,” said Clay Semenkovich, who studies insulin resistance and diabetes at Washington University in St. Louis but was not involved in the work. “This paper addresses, with an experimental model, a serious problem: that type 1 diabetes is increasing at an alarming rate.”
In type 1 diabetes, the immune system destroys cells in the pancreas, rendering patients unable to regulate blood glucose without taking insulin. Incidence of the autoimmune disease, which usually affects children, has been doubling every 20 to 25 years, study coauthor Martin Blaser of New York University School of Medicine told The Scientist.
Blaser’s team has found evidence to suggest disturbance in the gut microbiome is in part to blame for this increase. Along with ...


















