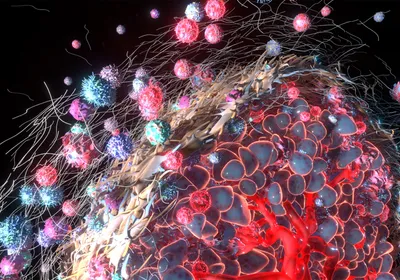
ABOVE: MODIFIED FROM
© Kailey whitman
In 2014, at Washington University School of Medicine in St. Louis, six melanoma patients received infusions of an anticancer vaccine composed of their own dendritic cells. Our WashU colleagues had extracted immune cells from the patients’ blood two months earlier, cultured them in the lab, and mixed in peptides selected and synthesized based on specific mutations present in the genomes of each patient’s tumor. The cells had then taken up the peptides much as they take up foreign antigens in the body in the course of normal immune patrol. When the clinical team administered the vaccines—each patient received three infusions over several months—they hoped that the dendritic cells would induce activation and expansion of T cells capable of identifying and destroying the cancer cells, while sparing healthy tissue.
This first test of personalized cancer vaccines in people grew out of our collaborative efforts to develop ...