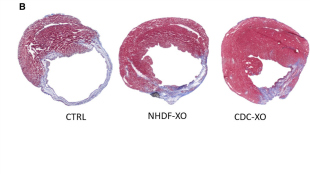
 Mouse hearts after a heart attack were injected with a vehicle (CTRL), exosomes from normal human dermal fibroblasts (NHDF-XO), or exosomes from cardiosphere-derived cells (CDC-XO).A.G.-E. Ibrahim et al., Stem Cell ReportsAn early-stage clinical trial, published in the Journal of the American College of Cardiology in January, showed that a certain type of stem cell injected into the human heart could help repair damage after a heart attack. But according to a mouse study published in Stem Cell Reports today (May 6), the cells themselves may be unnecessary. Rather, exosomes—tiny, lipid-bound vesicles secreted by the stem cells—appear to be the essential ingredient for healing injured cardiac tissue.
Mouse hearts after a heart attack were injected with a vehicle (CTRL), exosomes from normal human dermal fibroblasts (NHDF-XO), or exosomes from cardiosphere-derived cells (CDC-XO).A.G.-E. Ibrahim et al., Stem Cell ReportsAn early-stage clinical trial, published in the Journal of the American College of Cardiology in January, showed that a certain type of stem cell injected into the human heart could help repair damage after a heart attack. But according to a mouse study published in Stem Cell Reports today (May 6), the cells themselves may be unnecessary. Rather, exosomes—tiny, lipid-bound vesicles secreted by the stem cells—appear to be the essential ingredient for healing injured cardiac tissue.
“This study is very exciting,” said Guo-Chang Fan, who studies exosomes at the University of Cincinnati but did not participate in the research. He added that the results open up the possibility of a “cell-free therapeutic strategy.”
The clinical trial to evaluate tissue repair after heart attack involved the autologous injection of certain cardiac stem cells, called cardiosphere-derived cells. So far, the study has shown that patients given the cells have had increases in living heart muscle and decreases in scar tissue, although it’s not clear yet whether these effects translate to any health benefits.
Eduardo Marbán, a cardiologist at the Cedars-Sinai Heart Institute in Los Angeles who led the clinical trial, had suspected that the responses to the cardiosphere-derived cells came from indirect mechanisms, ...