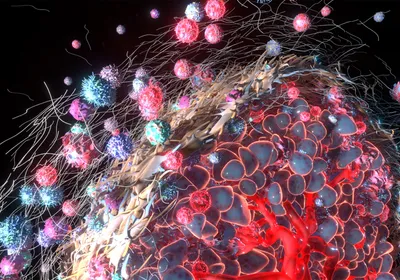
ISTOCK, ALENGO
ISTOCK, ALENGO
Ethic guidelines drastically limit experiments on human subjects. Hence, the fundamental mechanisms of human diseases are mostly studied in vitro or in animal models. These are only substitutes for understanding human physiology and disease. Proving that a mechanism responsible for disease progression in a model system is also relevant to human diseases—not to mention then translating it into a new therapeutic—is a major bottleneck in biomedicine. In the end, only clinical interventions on human will bridge models and human disease.
One approach is to look for correlations. If you can show that patients with tumors expressing, for example, stem cell markers have a much worse prognosis than those without them, that would suggest that stem cells are involved in human disease progression. This line of ...