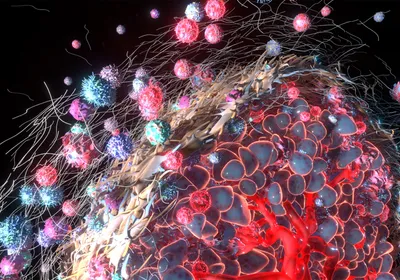
Evidence from the clinic and research labs in the last couple of decades shows that there is no single cure for cancer. Within a group of patients, individuals with what look to be identical tumor types react to the same treatment very differently. This often results in a waste of time and quality of life for those that don’t respond, and it has impeded cancer treatment development for years. As a result, precision oncology, the molecular profiling of tumors to identify patient-specific treatments, has become a necessary tool in the battle against cancer.
Recently, researchers developed in vitro patient-derived cell models to guide personalized care in cancer.1 “The challenge is to make a platform technology that can truly be used in the clinic, and to be very reproducible, fast, and scalable,” said Xiling Shen, a professor in biomedical engineering at Duke University. While training to be an electrical engineer, Shen ...