 © ISTOCK.COM/TTSZBecause age is the largest risk factor for cancer, as the life expectancy of the world’s population continues to increase, cancer incidence is projected to rise dramatically. A 2011 report on Global Health and Aging released by the National Institutes of Health and World Health Organization predicts a tripling of the number of people aged 65 or older to 1.5 billion by 2050, and the annual number of new cancer cases is projected to reach 27 million by 2030. Undoubtedly, alleviating the diseases and disabilities associated with an aging global population will require the development of new anticancer approaches to avoid economic and humanitarian calamities.
© ISTOCK.COM/TTSZBecause age is the largest risk factor for cancer, as the life expectancy of the world’s population continues to increase, cancer incidence is projected to rise dramatically. A 2011 report on Global Health and Aging released by the National Institutes of Health and World Health Organization predicts a tripling of the number of people aged 65 or older to 1.5 billion by 2050, and the annual number of new cancer cases is projected to reach 27 million by 2030. Undoubtedly, alleviating the diseases and disabilities associated with an aging global population will require the development of new anticancer approaches to avoid economic and humanitarian calamities.
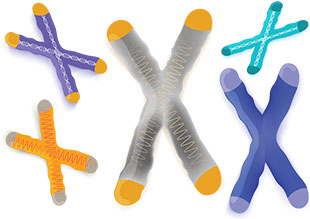
Cellular immortality is a hallmark of cancers that distinguishes them from normal tissue. Every time a normal somatic cell divides, the DNA at the ends of its chromosomes, called the telomeres, gets shorter. When the telomeres shorten too much, an alarm signal is generated, and the cell permanently stops dividing and enters senescence or undergoes apoptosis. Telomere shortening thus acts as a biological mechanism for limiting cellular life span. Cancer cells, on the other hand, can become immortalized by activating a telomere maintenance mechanism (TMM) that counteracts telomere shortening by synthesizing new telomeric DNA from either an RNA template using the enzyme telomerase or a DNA template using a mechanism called alternative lengthening of telomeres (ALT).
Because the presence of a TMM is an almost ...