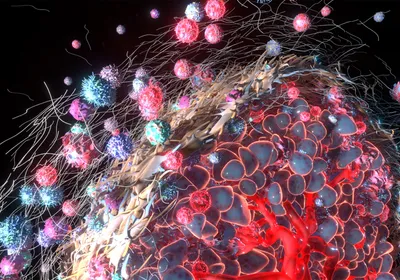
Fluorescent CLR1501 in pancreatic cancer cellsWEICHERT ET AL.The compounds: Phospholipid ethers (PLEs) are naturally occurring molecules that accumulate in the membranes of cancer cells, but not healthy cells. Using radioactive and fluorescent analogs of PLEs, scientists at the University of Wisconsin and from the firm Cellectar Biosciences, both in Madison, are now tracking and treating tumors in animals and patients. Their findings are reported today (June 11) in Science Translational Medicine.
Fluorescent CLR1501 in pancreatic cancer cellsWEICHERT ET AL.The compounds: Phospholipid ethers (PLEs) are naturally occurring molecules that accumulate in the membranes of cancer cells, but not healthy cells. Using radioactive and fluorescent analogs of PLEs, scientists at the University of Wisconsin and from the firm Cellectar Biosciences, both in Madison, are now tracking and treating tumors in animals and patients. Their findings are reported today (June 11) in Science Translational Medicine.
“They’ve identified a type of lipid that is usually expressed by cancers but not by normal cells and they’ve taken advantage of this observation,” said Jeremy Rich from the Cleveland Clinic Lerner Research Institute in Ohio, who was not involved in the work.
Although researchers have known for more than 40 years that PLEs accumulate in cancer cells, it is not clear why. “Normal cells seem to metabolize them [PLEs] . . . break them down and eliminate them,” said John Kuo, a professor of neurological surgery and human oncology at the University of Wisconsin, who led the study. For some reason, that metabolic process appears to be amiss in most cancer cells. “Maybe because they’re dividing so quickly they just don’t dot their Is ...