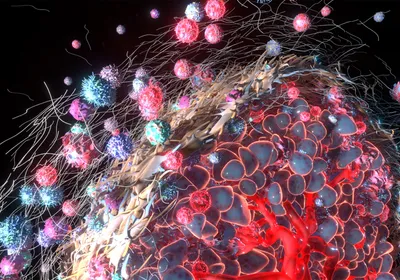
Melanoma metastasis in vivo, visualized using MetAlert mice. The image on the right is an animal that emits bioluminescence upon the induction of new lymphatic vessels, an early stage in the development of metastasis. On the left is an equivalent animal with non-aggressive melanoma.MARISOL SOENGAS/CNIOMetastasizing cancer cells travel through the lymphatic vasculature, but it’s not clear what role the formation of lymph vessels, called lymphangiogenesis, plays in cancer progression. Now, an international team of researchers has used a new mouse model to link lymphangiogenesis to melanoma metastasis. Bioluminescent cells in the animals not only showed where tumors were spreading, but after tumor removal could indicate that cancer recurrence was imminent. Their findings were published today (June 28) in Nature.
Melanoma metastasis in vivo, visualized using MetAlert mice. The image on the right is an animal that emits bioluminescence upon the induction of new lymphatic vessels, an early stage in the development of metastasis. On the left is an equivalent animal with non-aggressive melanoma.MARISOL SOENGAS/CNIOMetastasizing cancer cells travel through the lymphatic vasculature, but it’s not clear what role the formation of lymph vessels, called lymphangiogenesis, plays in cancer progression. Now, an international team of researchers has used a new mouse model to link lymphangiogenesis to melanoma metastasis. Bioluminescent cells in the animals not only showed where tumors were spreading, but after tumor removal could indicate that cancer recurrence was imminent. Their findings were published today (June 28) in Nature.
“The question is, how do cancer cells get to the visceral metastasis sites, [such as] lung and liver?” Harvard University cancer biologist Rakesh Jain, who did not participate in the work, tells The Scientist. “This paper indicates that lymphangiogenesis plays an important role in distal metastasis. It’s a very nice story.”
Marisol Soengas, who leads the melanoma group at the Spanish National Cancer Research Centre in Madrid, wanted to investigate the early stages of metastasis in cutaneous melanoma, an especially aggressive form of cancer. “When the metastases occur, they are not just a single metastasis,” Soengas says. Instead, “the cells tend to disseminate to different organs in the body and develop what we call multiple metastases. That’s a complication in trying to visualize the process ...