 CHRIS BICKEL, AAAS CRISPR-Cas9 gene editing can extend survival in a mouse model of amyotrophic lateral sclerosis (ALS), a fatal neurodegenerative disease, according to a study published yesterday (December 20) in Science Advances.
CHRIS BICKEL, AAAS CRISPR-Cas9 gene editing can extend survival in a mouse model of amyotrophic lateral sclerosis (ALS), a fatal neurodegenerative disease, according to a study published yesterday (December 20) in Science Advances.
“The treatment did not make the ALS mice normal and it is not yet a cure,” study coauthor David Schaffer, a professor of chemical and biomolecular engineering at the University of California, Berkeley, says in a press release. “But based upon what I think is a really strong proof of concept, CRISPR-Cas9 could be a therapeutic molecule for ALS.”
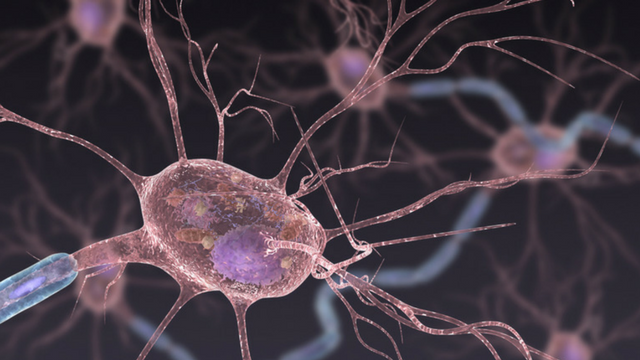
ALS, or Lou Gehrig’s disease, affects some 20,000 Americans and is characterized by the premature death of motor neurons in the brain stem and spinal cord. The disease causes progressive muscle deterioration and eventually results in paralysis and death. There are no available treatments to delay the muscle wasting and currently approved drugs can extend survival by a few months at most.
Schaffer and his colleagues ...





















